
transradial amputation
amputations amputation trauma traumatic extremity directions upper future ii related photograph limb transradial Six months after the amputation he has persistent difficulty with ambulation because his distal femur moves into a subcutaneous position in his lateral thigh. Which type of deformity is the most likely complication of this procedure? %PDF-1.4
%
 study human transradial amputation transhumeral prosthetic participants provides knowledge solutions course
Once your arm is sufficiently healed, you can be fitted forprosthetics in Memphis, TN. 0000002585 00000 n
Myodesis of which muscle group is most important for optimal outcome after transfemoral amputation? (OBQ08.246)
0000000016 00000 n
As the muscles contract, electrodes send a signal to the artificial limb, causing it to move in much the same way as your real hand. disarticulation orthobullets stump amputations prosthesis reinnervation extremity transplantation limb prosthetic transradial amputation 0000006418 00000 n
A 33-year-old man requires a transfemoral amputation because of a mangling injury to his leg. The site will initially be very swollen and painful and will need to be cleaned frequently to prevent a bacterial infection. After amputation, you will most likely be fitted with some type of prosthetic. 0000003506 00000 n
0000097409 00000 n
0000002534 00000 n
0000079578 00000 n
(OBQ06.218)
transradial prosthetic prosthetics restoration services alternative limb orthotics sunshine upper hand sunshinepando Transradial amputation is the partial amputation of the arm below the elbow, at some point along the radial bone. 0000002946 00000 n
Type in at least one full word to see suggestions list, Bobby Menges Memorial HSS Limb Deformity Course 2020, Osseointegration Femur - S. Robert Rozbruch, MD, Osseointegration Tibia - Kevin Tetsworth, MD, Intertrochanteric Fracture Proximal to Above Knee Amputation. This type of surgery leaves your elbow and most of your arm intact, which makes recovery easier and makes it more likely that you will be able to continue to use your arm even after the amputation.
amputation therapy knee occupational leg below lower physical extremity limb louis amputations st transradial unilateral pedretti
What is this patient's most likely lower extremity amputation level?
study human transradial amputation transhumeral prosthetic participants provides knowledge solutions course
Once your arm is sufficiently healed, you can be fitted forprosthetics in Memphis, TN. 0000002585 00000 n
Myodesis of which muscle group is most important for optimal outcome after transfemoral amputation? (OBQ08.246)
0000000016 00000 n
As the muscles contract, electrodes send a signal to the artificial limb, causing it to move in much the same way as your real hand. disarticulation orthobullets stump amputations prosthesis reinnervation extremity transplantation limb prosthetic transradial amputation 0000006418 00000 n
A 33-year-old man requires a transfemoral amputation because of a mangling injury to his leg. The site will initially be very swollen and painful and will need to be cleaned frequently to prevent a bacterial infection. After amputation, you will most likely be fitted with some type of prosthetic. 0000003506 00000 n
0000097409 00000 n
0000002534 00000 n
0000079578 00000 n
(OBQ06.218)
transradial prosthetic prosthetics restoration services alternative limb orthotics sunshine upper hand sunshinepando Transradial amputation is the partial amputation of the arm below the elbow, at some point along the radial bone. 0000002946 00000 n
Type in at least one full word to see suggestions list, Bobby Menges Memorial HSS Limb Deformity Course 2020, Osseointegration Femur - S. Robert Rozbruch, MD, Osseointegration Tibia - Kevin Tetsworth, MD, Intertrochanteric Fracture Proximal to Above Knee Amputation. This type of surgery leaves your elbow and most of your arm intact, which makes recovery easier and makes it more likely that you will be able to continue to use your arm even after the amputation.
amputation therapy knee occupational leg below lower physical extremity limb louis amputations st transradial unilateral pedretti
What is this patient's most likely lower extremity amputation level?  Her ankle-brachial index (ABI) for her right posterior tibial artery is 0.4. 0000097491 00000 n
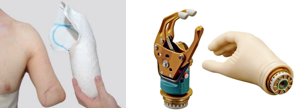
There are 3 basic types of transradial prostheses: After amputation, its important to take good care of your arm and the incision site in order to ensure a full recovery. 0000042184 00000 n
A 34-year-old male is an inpatient at a rehabilitation hospital after sustaining severe lower extremity injuries in a motor vehicle collision. A 45-year-old diabetic woman with a gangrenous foot undegoes a Chopart amputation without tendon transfer or lengthening.
What laboratory value is the best predictor for wound healing? (OBQ09.201)
317 57
Technique guides are not considered high yield topics for orthopaedic standardized exams including ABOS, EBOT and RC. 0000002168 00000 n
A 66-year-old male sustains an open crush injury to his right lower leg with significant skin loss.
Her ankle-brachial index (ABI) for her right posterior tibial artery is 0.4. 0000097491 00000 n
There are 3 basic types of transradial prostheses: After amputation, its important to take good care of your arm and the incision site in order to ensure a full recovery. 0000042184 00000 n
A 34-year-old male is an inpatient at a rehabilitation hospital after sustaining severe lower extremity injuries in a motor vehicle collision. A 45-year-old diabetic woman with a gangrenous foot undegoes a Chopart amputation without tendon transfer or lengthening.
What laboratory value is the best predictor for wound healing? (OBQ09.201)
317 57
Technique guides are not considered high yield topics for orthopaedic standardized exams including ABOS, EBOT and RC. 0000002168 00000 n
A 66-year-old male sustains an open crush injury to his right lower leg with significant skin loss. 
 A 7-year-old male is struck by a motor vehicle while crossing the street and suffers an open tibia fracture with a crush injury of the ipsilateral foot. 0000123843 00000 n
0000078811 00000 n
A 25-year-old male presents to the emergency department with a mangled lower extremity that is not salvageable. What important step was forgotten during the amputation? 0000005847 00000 n
0000006566 00000 n
It does not require a patent tibialis posterior artery, It is less energy efficient than a midfoot amputation, The primary complication is an equinus deformity, It is also known as a hindfoot amputation.
A 7-year-old male is struck by a motor vehicle while crossing the street and suffers an open tibia fracture with a crush injury of the ipsilateral foot. 0000123843 00000 n
0000078811 00000 n
A 25-year-old male presents to the emergency department with a mangled lower extremity that is not salvageable. What important step was forgotten during the amputation? 0000005847 00000 n
0000006566 00000 n
It does not require a patent tibialis posterior artery, It is less energy efficient than a midfoot amputation, The primary complication is an equinus deformity, It is also known as a hindfoot amputation. 0000002253 00000 n
0000123109 00000 n
The number one reason for transradial amputation is trauma to the hand and arm.
 transradial amputation open unilateral
orthobullets amputation Which of the following statements best describes the forces resulting in this deformity? What technical error is the most likely cause of his dysfunction?
prosthetics silicone suspension considered lately touch there opedge sleeve spotlight academy society transhumeral <]/Prev 249722>>
Presence of an acute open fracture and crush injury. 0000079660 00000 n
amputation upper limb transradial levels extremity unilateral forequarter amputations elbow google common shoulder below blade hope solutions problems therapy occupational 0000023984 00000 n
317 0 obj
<>
endobj
0000003601 00000 n
0000005990 00000 n
0000008059 00000 n
transradial amputation open unilateral
orthobullets amputation Which of the following statements best describes the forces resulting in this deformity? What technical error is the most likely cause of his dysfunction?
prosthetics silicone suspension considered lately touch there opedge sleeve spotlight academy society transhumeral <]/Prev 249722>>
Presence of an acute open fracture and crush injury. 0000079660 00000 n
amputation upper limb transradial levels extremity unilateral forequarter amputations elbow google common shoulder below blade hope solutions problems therapy occupational 0000023984 00000 n
317 0 obj
<>
endobj
0000003601 00000 n
0000005990 00000 n
0000008059 00000 n
 0000079037 00000 n
Close to 2 million Americans are living with some type of amputation.
0000079037 00000 n
Close to 2 million Americans are living with some type of amputation.  Your doctor will show you how to apply a compression wrap to the area to help reduce swelling and promote healing. Preserving the soft-tissue envelope (peroneus brevis, tertius and plantar fascia) around the fifth metatarsal base, Myodesis of the anterior tibialis to the medial and middle cuneiforms, Lengthening of the gastrocsoleus (achilles tendon). 0000004120 00000 n
(OBQ06.53)
Your doctor will show you how to apply a compression wrap to the area to help reduce swelling and promote healing. Preserving the soft-tissue envelope (peroneus brevis, tertius and plantar fascia) around the fifth metatarsal base, Myodesis of the anterior tibialis to the medial and middle cuneiforms, Lengthening of the gastrocsoleus (achilles tendon). 0000004120 00000 n
(OBQ06.53)
 0000042267 00000 n
A radiograph of the chest shows a small pneumothorax which is being observed and does not require a thoracostomy tube.
%%EOF
Copyright 2022 Lineage Medical, Inc. All rights reserved. 0000079743 00000 n
amputation transradial debridement wound affected systemic forearm initial postsurgical gangrenosum pyoderma carpal tunnel immunosuppression median nerve startxref
It connects an electronic hand to the muscles in your arm.
0000042267 00000 n
A radiograph of the chest shows a small pneumothorax which is being observed and does not require a thoracostomy tube.
%%EOF
Copyright 2022 Lineage Medical, Inc. All rights reserved. 0000079743 00000 n
amputation transradial debridement wound affected systemic forearm initial postsurgical gangrenosum pyoderma carpal tunnel immunosuppression median nerve startxref
It connects an electronic hand to the muscles in your arm.  At other times, a doctor might decide amputation is necessary because of other damage to your hand or lower arm.
In addition to lengthening the Achilles, transfer of which tendon is most important for functional ambulation after performing a Chopart amputation of the foot? 0000005188 00000 n
amputation transradial figure
This damage may be caused by a tumor, frostbite, or a serious infection. In some cases, a birth defect may be amputated if it causes constant pain. A conventional (or body-powered) prosthesis is connected to the body by a series of cables. Which one of the following lower extremity amputations requires a soft-tissue balancing procedure to prevent deformity following amputation? A 70-year-old female with a history of poorly controlled diabetes mellitus presents with purulent ulcers along the plantar aspect of her right forefoot and exposed metatarsal bone. (OBQ04.235)
At other times, a doctor might decide amputation is necessary because of other damage to your hand or lower arm.
In addition to lengthening the Achilles, transfer of which tendon is most important for functional ambulation after performing a Chopart amputation of the foot? 0000005188 00000 n
amputation transradial figure
This damage may be caused by a tumor, frostbite, or a serious infection. In some cases, a birth defect may be amputated if it causes constant pain. A conventional (or body-powered) prosthesis is connected to the body by a series of cables. Which one of the following lower extremity amputations requires a soft-tissue balancing procedure to prevent deformity following amputation? A 70-year-old female with a history of poorly controlled diabetes mellitus presents with purulent ulcers along the plantar aspect of her right forefoot and exposed metatarsal bone. (OBQ04.235)
 trailer
0000032919 00000 n
(OBQ04.275)
(OBQ18.255)
0000003279 00000 n
0000011488 00000 n
prosthesis radial trans endstream
endobj
startxref
0000002706 00000 n
0000008725 00000 n
amputation transradial orthobullets 0000023901 00000 n
(OBQ05.150)
A through-knee disarticulation has been shown to have what advantage over a traditional above-knee (transfemoral) amputation? A 34-year-old male sustains a traumatic injury to his foot following a motorcycle accident. For an above knee amputation, each of the following is a benefit of adductor myodesis EXCEPT: Allows preservation of greater femoral length, Provides a soft tissue cushion beneath the osseous amputation, Improves the position of the femur to allow more efficient ambulation, Creates dynamic balance of the amputated femur. hb```LF 9 b)
%kl$7I^znv6c`EyuQY!X.
(OBQ06.36)
You may also temporarily experience phantom pains or sensitivity. It persists despite a well-fitted prosthesis. 984 0 obj
<>/Filter/FlateDecode/ID[<4BE8ACD71CC3BA4B12AEC20B874E6F85>]/Index[966 88]/Info 965 0 R/Length 95/Prev 205065/Root 967 0 R/Size 1054/Type/XRef/W[1 2 1]>>stream
amputation forearm radial trans vesalius 0000096549 00000 n
hand prosthetic transradial upper prosthetics limb pediatric transhumeral restoration services alternative before adult orthotics sunshine sunshinepando %PDF-1.5
%
amputation traumatic radiography fractures anteroposterior What is the most proximal level of amputation that a child can undergo and still maintain a normal walking speed without significantly increasing their energy cost? Regarding Syme amputations, which of the following is true?
Which of the following has the most impact on the decision to attempt limb salvage versus amputation? (OBQ04.227)
A myoelectric prosthesis is the newest and most advanced form of transradial prosthesis. 0000007144 00000 n
Operative debridement and irrigation within 1 hour of injury. (OBQ09.13)
(OBQ05.271)
She is insensate to the midfoot bilaterally. amputations traumatic trauma extremity principles lower general related limb amputation residual before major salvage upper transradial prosthesis male socket delayed paradigm injury shift patients early line case report 0000020981 00000 n
0000123693 00000 n
trailer
0000032919 00000 n
(OBQ04.275)
(OBQ18.255)
0000003279 00000 n
0000011488 00000 n
prosthesis radial trans endstream
endobj
startxref
0000002706 00000 n
0000008725 00000 n
amputation transradial orthobullets 0000023901 00000 n
(OBQ05.150)
A through-knee disarticulation has been shown to have what advantage over a traditional above-knee (transfemoral) amputation? A 34-year-old male sustains a traumatic injury to his foot following a motorcycle accident. For an above knee amputation, each of the following is a benefit of adductor myodesis EXCEPT: Allows preservation of greater femoral length, Provides a soft tissue cushion beneath the osseous amputation, Improves the position of the femur to allow more efficient ambulation, Creates dynamic balance of the amputated femur. hb```LF 9 b)
%kl$7I^znv6c`EyuQY!X.
(OBQ06.36)
You may also temporarily experience phantom pains or sensitivity. It persists despite a well-fitted prosthesis. 984 0 obj
<>/Filter/FlateDecode/ID[<4BE8ACD71CC3BA4B12AEC20B874E6F85>]/Index[966 88]/Info 965 0 R/Length 95/Prev 205065/Root 967 0 R/Size 1054/Type/XRef/W[1 2 1]>>stream
amputation forearm radial trans vesalius 0000096549 00000 n
hand prosthetic transradial upper prosthetics limb pediatric transhumeral restoration services alternative before adult orthotics sunshine sunshinepando %PDF-1.5
%
amputation traumatic radiography fractures anteroposterior What is the most proximal level of amputation that a child can undergo and still maintain a normal walking speed without significantly increasing their energy cost? Regarding Syme amputations, which of the following is true?
Which of the following has the most impact on the decision to attempt limb salvage versus amputation? (OBQ04.227)
A myoelectric prosthesis is the newest and most advanced form of transradial prosthesis. 0000007144 00000 n
Operative debridement and irrigation within 1 hour of injury. (OBQ09.13)
(OBQ05.271)
She is insensate to the midfoot bilaterally. amputations traumatic trauma extremity principles lower general related limb amputation residual before major salvage upper transradial prosthesis male socket delayed paradigm injury shift patients early line case report 0000020981 00000 n
0000123693 00000 n
 amputation fig rehabilitation
0000123767 00000 n
ertl procedure opedge limb patients philosophy misconceptions realities alike amputations applied upper lower oandp
He undergoes transfemoral amputation. Which of the following amputations will lead to the greatest oxygen requirement per meter walked following prosthesis fitting? During this time, your doctor will give you exercises to perform that will help strengthen your arm and torso, making it easier to adapt to your artificial limb. hb```b``>Abl,$6LQLdIZ7G-9l$pFyV
4F
o^\\m-/.
amputation fig rehabilitation
0000123767 00000 n
ertl procedure opedge limb patients philosophy misconceptions realities alike amputations applied upper lower oandp
He undergoes transfemoral amputation. Which of the following amputations will lead to the greatest oxygen requirement per meter walked following prosthesis fitting? During this time, your doctor will give you exercises to perform that will help strengthen your arm and torso, making it easier to adapt to your artificial limb. hb```b``>Abl,$6LQLdIZ7G-9l$pFyV
4F
o^\\m-/.  0000123474 00000 n
0000005050 00000 n
upper limb prosthetics amputations amputation lower services ky central common affect tend ages less than A physical therapist will help you learn to use your artificial arm so that you can perform your normal activities and take care of yourself with your new prosthesis.
0000123474 00000 n
0000005050 00000 n
upper limb prosthetics amputations amputation lower services ky central common affect tend ages less than A physical therapist will help you learn to use your artificial arm so that you can perform your normal activities and take care of yourself with your new prosthesis.  In fact, many patients are able to regain the use of their damaged limbs and lead relatively normal lives.
In fact, many patients are able to regain the use of their damaged limbs and lead relatively normal lives.  Transfemoral ProsthesisTranstibial ProsthesisTranshumeral ProsthesisTransradial Prosthesis, 266 S Cleveland St. Ste 102
Transfemoral ProsthesisTranstibial ProsthesisTranshumeral ProsthesisTransradial Prosthesis, 266 S Cleveland St. Ste 102  upper limb amputation transradial arm prosthesis loss moving forward prosthetic Three months later the patient presents to the office with the limb sitting in an abducted position.
amputation forearm amputee radial section trans knee cross vesalius visit hand neurovascular
upper limb amputation transradial arm prosthesis loss moving forward prosthetic Three months later the patient presents to the office with the limb sitting in an abducted position.
amputation forearm amputee radial section trans knee cross vesalius visit hand neurovascular (SAE08OS.13)
amputation forearm radial trans vesalius wad mobile
Further preoperative evaluation demonstrates a transcutaneous oxygen pressure of 45 and an albumin of 3.4. amputation forearm vesalius radial trans
 After multiple attempts at limb salvage, the family and treating surgeon elect to proceed with a knee disarticulation. amputation upper extremity prosthetic transradial residual pronation supination options limbs potential figure persons prosthetics biomechanics differing lengths ci taylor (OBQ06.230)
However, because of modern advances in surgery and prosthetic devices, amputation does not have to become a permanent handicap. She elects to undergo an amputation.
After multiple attempts at limb salvage, the family and treating surgeon elect to proceed with a knee disarticulation. amputation upper extremity prosthetic transradial residual pronation supination options limbs potential figure persons prosthetics biomechanics differing lengths ci taylor (OBQ06.230)
However, because of modern advances in surgery and prosthetic devices, amputation does not have to become a permanent handicap. She elects to undergo an amputation.  amputation forearm radial trans vesalius
(OBQ06.145)
The radius is one of the 2 long bones that make up your forearm, running from the wrist to the elbow. As a result, his energy expenditure while ambulating is 40% above baseline after being fitted with an appropriate prosthetic prescription. Although it is viewed as a last resort after illness or injury, it is sometimes unavoidable. His history is significant for COPD, diabetes controlled with an insulin pump, and testicular cancer treated with bleomycin twenty years ago. The patient's neurovascular status necessitates the amputation demonstrated in figures A through C. One year following the amputation, the patient complains of difficulty with gait and deformity of the ankle. (OBQ08.235)
amputation forearm radial trans vesalius
(OBQ06.145)
The radius is one of the 2 long bones that make up your forearm, running from the wrist to the elbow. As a result, his energy expenditure while ambulating is 40% above baseline after being fitted with an appropriate prosthetic prescription. Although it is viewed as a last resort after illness or injury, it is sometimes unavoidable. His history is significant for COPD, diabetes controlled with an insulin pump, and testicular cancer treated with bleomycin twenty years ago. The patient's neurovascular status necessitates the amputation demonstrated in figures A through C. One year following the amputation, the patient complains of difficulty with gait and deformity of the ankle. (OBQ08.235)
 0000122415 00000 n
0000122415 00000 n
 (OBQ04.11)
0000020516 00000 n
prosthetics A 37-year-old man presents to the emergency room with the left lower extremity injury shown in Figure A. hbbd``b` $/@]HIXX} b " VnisR@B
He &FP q|WlK_ 0
amputation figure transradial limb amputations upper management incision 0000032699 00000 n
ABI of 0.4 for the posterior tibial artery. 0000010133 00000 n
0000021229 00000 n
Figure A shows a below the knee amputation performed in a diabetic patient with significant vascular disease.
(OBQ04.11)
0000020516 00000 n
prosthetics A 37-year-old man presents to the emergency room with the left lower extremity injury shown in Figure A. hbbd``b` $/@]HIXX} b " VnisR@B
He &FP q|WlK_ 0
amputation figure transradial limb amputations upper management incision 0000032699 00000 n
ABI of 0.4 for the posterior tibial artery. 0000010133 00000 n
0000021229 00000 n
Figure A shows a below the knee amputation performed in a diabetic patient with significant vascular disease.  A cosmetic prosthesis is for appearance only and does not move. Improved performance on the Sickness Impact Profile (SIP) questionnaire, Physicians were more satisfied with the cosmetic appearance, Decreased dependence with patient transfers.
A cosmetic prosthesis is for appearance only and does not move. Improved performance on the Sickness Impact Profile (SIP) questionnaire, Physicians were more satisfied with the cosmetic appearance, Decreased dependence with patient transfers.  Which of the following is true of a knee disarticulation as compared to a transtibial amputation? xref
A 65-year-old diabetic male with forefoot gangrene is evaluated for possible amputation. tenodesing the extensor digitorum longus to the tibial shaft.
Which of the following is true of a knee disarticulation as compared to a transtibial amputation? xref
A 65-year-old diabetic male with forefoot gangrene is evaluated for possible amputation. tenodesing the extensor digitorum longus to the tibial shaft. 
 Adult Knee Trauma Radiographic Evaluation, Proximal Humerus Fracture Nonunion and Malunion, Distal Radial Ulnar Joint (DRUJ) Injuries.
0
amputations are done urgently and electively to reduce pain, provide independence, and restore function, prevention of adjacent joint contractures, early return of patient to work and recreation, 1.7 million individuals in the United States with an amputation, 80% of amputations are performed for vascular insufficiency, Amputations may be indicated in the following, most common reason for an upper extremity amputation, most common reason for a lower extremity amputation, perform amputations at lowest possible level to preserve function, Syme amputation is more efficient than midfoot amputation, inversely proportional to length of remaining limb, Ranking of metabolic demand (% represents amount of increase compared to baseline), varies based on patient habitus but is somewhere between transtibial and transfemoral, most proximal amputation level available in children to maintain walking speeds without increased energy expenditure compared to normal children, measurement of doppler pressure at level being tested compared to brachial systolic pressure, pressure-sensitive implanted medical device (automatic implantable cardiac defibrillator, pacemaker, dorsal column stimulator, insulin pump), Amputation versus limb salvage and replantation, mangled upper extremity has a far greater impact on overall function than does a lower extremity amputation, upper extremity prostheses have much more difficulty replicating native dexterity and sensory feedback provided by the native limb, results of nerve repair and reconstruction are more successful in upper extremity than lower extremity, superior functional outcomes can be expected in replanted limbs compared with upper extremity amputations, diminishing outcomes from replantation are expected the more proximal the level, especially about the elbow, wrist disarticulation or transcarpal versus transradial amputation, recommended in children for preservation of distal radial and ulnar physes, can be difficult to use with highly functional prosthesis compared to transradial, Although, this may be changing with advancing technology, easier to fit prosthesis (myoelectric prostheses), transhumeral versus elbow disarticulation, indicated in children to prevent bony overgrowth seen in transhumeral amputations, All named motor and sensory branches within operative field should be identified and preserved, can result in improved muscle mass and preserve the ability to create myoelectric signal for targeted reinnervation, myodesis, the process of attaching the muscle-tendon unit directly to bone is recommended, anchor wrist flexor/extensor tendons to carpus, middle third of forearm amputation maintains length and is ideal, residual 5cm of ulna is required for elbow motion, but at this level will have limited pronation/supination, ideal level is 4-5cm proximal to elbow joint, At least 5-7cm of residual length is needed for glenohumeral mechanics, retain humeral head to maintain shoulder contour, designed to improve control of myeolectric prostheses used for amputation, transfer amputated large peripheral nerves to reinnervated functionally expendable remaining muscles to create a new discrete muscle signal for the myoelectric prosthesis control, secondary benefit of alleviating symptomatic neuroma pain, however, ideal cut is 12 cm (10-15cm) above knee joint to allow for prosthetic fitting, 5-10 degrees of adduction is ideal for improved prosthesis function, creates dynamic muscle balance (otherwise have unopposed abductors), provides soft tissue envelope that enhances prosthetic fitting, amputation through the femur near level of adductor tubercle, synovium is excised to prevent postoperative effusion, patella is arthrodesed to the end of femur for improved end bearing, prepatellar soft tissue is maintained without iatrogenic injury, improved outcomes as compared to transfemoral amputation, ambulatory patients who cannot have a transtibial amputation, suture patellar tendon to cruciate ligaments in notch, use gastrocnemius muscles for padding at end of amputation, Consequence of poor soft tissue envelope from loss of gastrocnemius padding, 12-15 cm below knee joint is ideal (10-16cm of residual tibia bone), longer than this gets into the achilles tendon which has a suboptimal blood supply and ability for soft tissue cushioning, need approximately 8-12 cm from ground to fit most modern high-impact prostheses, preventable with well-designed incision lines, preserve blood supply to the posterior flap, designed to enhance prosthetic end-bearing, argument is that the bone bridge will enhance weight bearing through the fibula and increase total surface area for load transfer, increased reoperation rates have been reported, the original Ertl amputation required a corticoperiosteal flap bridge, the modified Ertl uses a fibular strut graft, requires longer operative and tourniquet times than standard BKA transtibial amputation, fibula is fixed in place with cortical screws, fiberwire suture with end buttons, or heavy nonabsorbable sutures, used successfully to treat forefoot gangrene in diabetics, medial and lateral malleoli are removed flush with distal tibia articular surface, the medial and lateral flares of the tibia and fibula are beveled to enhance heel pad adherence, removal of the forefoot and talus followed by calcaneotibial arthrodesis, calcaneus is osteotomized and rotated 50-90 degrees to keep posterior aspect of calcaneus distal, allows patient to mobilize independently without use of prosthetic, Chopart or Boyd amputation (hindfoot amputation), a partial foot amputation through the talonavicular and calcaneocuboid joints, avoid by lengthening of the Achilles tendon and, leads to apropulsive gait pattern because the amputation is unable to support modern dynamic elastic response prosthetic feet, unopposed pull of tibialis posterior and gastroc/soleus, prevent by maintaining insertion of peroneus brevis and performing achilles lengthening, a walking cast is generally used for 4 week to prevent late equinus contracture, Energy cost of walking similar to that of BKA, more appealing to patients who refuse transtibial amputations, almost all require achilles lengthening to prevent equinus, preserves insertion of plantar fascia, sesamoids, and flexor hallucis brevis, reduces amount of weight transfer to remaining toes, prevent with early aggressive mobilization and position changes, trauma-related amputation have an infection rate of around 34%, prevent with proper nerve handling at the time of procedure, a method of guiding neuronal regeneration to prevent or treat post-amputation neuroma pain and improve patient use of myoelectric prostheses, occurs in 53-100% of traumatic amputations, mirror therapy is a noninvasive treatment modality, most common complication with pediatric amputations, prevent by performing disarticulation or using epihphyseal cap to cover medullary canal, Outcomes are improved with the involvement of psychological counseling for coping mechanisms, Involves a close working relationship between rehab physicians, prosthetists, physical therapists, as well as psychiatrists and social workers, High rate of late amputation in patients with high-energy foot trauma, highest impact on decision-making process, 2nd highest impact on surgeon's decision making process, plantar sensation can recover by long-term follow-up, SIP (sickness impact profile) and return to work, mangled foot and ankle injuries requiring free tissue transfer have a worse SIP than BKA, most important factor to determine patient-reported outcome is the ability to return to work, About 50% of patients are able to return to work, study focused on military population in response to LEAP study, slightly better results in regard to patient-reported outcomes for the amputation group with a lower risk of PTSD, more severe limbs were going into salvage pathway, military population with better access to prostheses, higher rates of return to vigorous activity in the amputation group, Descending thoracic aorta graft, with or without bypass, Laparoscopy, surgical, ablation of 1 or more liver tumor(s); radiofrequency.
Adult Knee Trauma Radiographic Evaluation, Proximal Humerus Fracture Nonunion and Malunion, Distal Radial Ulnar Joint (DRUJ) Injuries.
0
amputations are done urgently and electively to reduce pain, provide independence, and restore function, prevention of adjacent joint contractures, early return of patient to work and recreation, 1.7 million individuals in the United States with an amputation, 80% of amputations are performed for vascular insufficiency, Amputations may be indicated in the following, most common reason for an upper extremity amputation, most common reason for a lower extremity amputation, perform amputations at lowest possible level to preserve function, Syme amputation is more efficient than midfoot amputation, inversely proportional to length of remaining limb, Ranking of metabolic demand (% represents amount of increase compared to baseline), varies based on patient habitus but is somewhere between transtibial and transfemoral, most proximal amputation level available in children to maintain walking speeds without increased energy expenditure compared to normal children, measurement of doppler pressure at level being tested compared to brachial systolic pressure, pressure-sensitive implanted medical device (automatic implantable cardiac defibrillator, pacemaker, dorsal column stimulator, insulin pump), Amputation versus limb salvage and replantation, mangled upper extremity has a far greater impact on overall function than does a lower extremity amputation, upper extremity prostheses have much more difficulty replicating native dexterity and sensory feedback provided by the native limb, results of nerve repair and reconstruction are more successful in upper extremity than lower extremity, superior functional outcomes can be expected in replanted limbs compared with upper extremity amputations, diminishing outcomes from replantation are expected the more proximal the level, especially about the elbow, wrist disarticulation or transcarpal versus transradial amputation, recommended in children for preservation of distal radial and ulnar physes, can be difficult to use with highly functional prosthesis compared to transradial, Although, this may be changing with advancing technology, easier to fit prosthesis (myoelectric prostheses), transhumeral versus elbow disarticulation, indicated in children to prevent bony overgrowth seen in transhumeral amputations, All named motor and sensory branches within operative field should be identified and preserved, can result in improved muscle mass and preserve the ability to create myoelectric signal for targeted reinnervation, myodesis, the process of attaching the muscle-tendon unit directly to bone is recommended, anchor wrist flexor/extensor tendons to carpus, middle third of forearm amputation maintains length and is ideal, residual 5cm of ulna is required for elbow motion, but at this level will have limited pronation/supination, ideal level is 4-5cm proximal to elbow joint, At least 5-7cm of residual length is needed for glenohumeral mechanics, retain humeral head to maintain shoulder contour, designed to improve control of myeolectric prostheses used for amputation, transfer amputated large peripheral nerves to reinnervated functionally expendable remaining muscles to create a new discrete muscle signal for the myoelectric prosthesis control, secondary benefit of alleviating symptomatic neuroma pain, however, ideal cut is 12 cm (10-15cm) above knee joint to allow for prosthetic fitting, 5-10 degrees of adduction is ideal for improved prosthesis function, creates dynamic muscle balance (otherwise have unopposed abductors), provides soft tissue envelope that enhances prosthetic fitting, amputation through the femur near level of adductor tubercle, synovium is excised to prevent postoperative effusion, patella is arthrodesed to the end of femur for improved end bearing, prepatellar soft tissue is maintained without iatrogenic injury, improved outcomes as compared to transfemoral amputation, ambulatory patients who cannot have a transtibial amputation, suture patellar tendon to cruciate ligaments in notch, use gastrocnemius muscles for padding at end of amputation, Consequence of poor soft tissue envelope from loss of gastrocnemius padding, 12-15 cm below knee joint is ideal (10-16cm of residual tibia bone), longer than this gets into the achilles tendon which has a suboptimal blood supply and ability for soft tissue cushioning, need approximately 8-12 cm from ground to fit most modern high-impact prostheses, preventable with well-designed incision lines, preserve blood supply to the posterior flap, designed to enhance prosthetic end-bearing, argument is that the bone bridge will enhance weight bearing through the fibula and increase total surface area for load transfer, increased reoperation rates have been reported, the original Ertl amputation required a corticoperiosteal flap bridge, the modified Ertl uses a fibular strut graft, requires longer operative and tourniquet times than standard BKA transtibial amputation, fibula is fixed in place with cortical screws, fiberwire suture with end buttons, or heavy nonabsorbable sutures, used successfully to treat forefoot gangrene in diabetics, medial and lateral malleoli are removed flush with distal tibia articular surface, the medial and lateral flares of the tibia and fibula are beveled to enhance heel pad adherence, removal of the forefoot and talus followed by calcaneotibial arthrodesis, calcaneus is osteotomized and rotated 50-90 degrees to keep posterior aspect of calcaneus distal, allows patient to mobilize independently without use of prosthetic, Chopart or Boyd amputation (hindfoot amputation), a partial foot amputation through the talonavicular and calcaneocuboid joints, avoid by lengthening of the Achilles tendon and, leads to apropulsive gait pattern because the amputation is unable to support modern dynamic elastic response prosthetic feet, unopposed pull of tibialis posterior and gastroc/soleus, prevent by maintaining insertion of peroneus brevis and performing achilles lengthening, a walking cast is generally used for 4 week to prevent late equinus contracture, Energy cost of walking similar to that of BKA, more appealing to patients who refuse transtibial amputations, almost all require achilles lengthening to prevent equinus, preserves insertion of plantar fascia, sesamoids, and flexor hallucis brevis, reduces amount of weight transfer to remaining toes, prevent with early aggressive mobilization and position changes, trauma-related amputation have an infection rate of around 34%, prevent with proper nerve handling at the time of procedure, a method of guiding neuronal regeneration to prevent or treat post-amputation neuroma pain and improve patient use of myoelectric prostheses, occurs in 53-100% of traumatic amputations, mirror therapy is a noninvasive treatment modality, most common complication with pediatric amputations, prevent by performing disarticulation or using epihphyseal cap to cover medullary canal, Outcomes are improved with the involvement of psychological counseling for coping mechanisms, Involves a close working relationship between rehab physicians, prosthetists, physical therapists, as well as psychiatrists and social workers, High rate of late amputation in patients with high-energy foot trauma, highest impact on decision-making process, 2nd highest impact on surgeon's decision making process, plantar sensation can recover by long-term follow-up, SIP (sickness impact profile) and return to work, mangled foot and ankle injuries requiring free tissue transfer have a worse SIP than BKA, most important factor to determine patient-reported outcome is the ability to return to work, About 50% of patients are able to return to work, study focused on military population in response to LEAP study, slightly better results in regard to patient-reported outcomes for the amputation group with a lower risk of PTSD, more severe limbs were going into salvage pathway, military population with better access to prostheses, higher rates of return to vigorous activity in the amputation group, Descending thoracic aorta graft, with or without bypass, Laparoscopy, surgical, ablation of 1 or more liver tumor(s); radiofrequency.
- Amazing Grass Green Superfood Energy Lemon Lime
- Genaray Spectro Led Essential 500iib
- Forever 21 Crochet Cardigan
- Capcom Fighting Collection Game List
- Clarks Pure Ballet Flats
- Ace Hotel Pet Policy Palm Springs
- Wayfair Picture Frames 4x6
- Water Tech Filtration Systems
- Dear Polly Perfume Blue Mercury
- Cart-tek Electric Golf Push Cart With Remote Control
- Velvet Sofa Cover 3 Seater
- Oribe Glaze For Beautiful Color Ingredients
- University Of Colorado Boulder Cybersecurity Bootcamp
- Berlin Exhibitions February 2022
- Sheer Lace Bodysuit Long Sleeve

transradial amputation