
how does covid-19 affect the blood
Is there anything you can do to reduce your risk for blood clots? In children and teens, this high inflammation is called multisystem inflammatory syndrome in children (MIS-C), and it can particularly affect the heart. Another possible side effect of COVID-19 is that it can lead to blood clots in some people. Of these people, 48 were in the ICU and 20 were not. Levi M, Thachil J, Iba T, Levy JH. The endothelial and immune cells add fuel to the fire, recruiting additional clotting factors and platelets, which help form clots. Can treatment for a rare blood disorder offset extreme immune responses to COVID-19? A new hypothesis suggests injury to blood vessels may drive some patients' deadly spiral into critical illness. Centers for Disease Control and Prevention. Your tax-deductible contribution plays a critical role in sustaining this effort. As fluid collects in your lungs, they carry less oxygen to your blood.  What should I expect?, UpToDate: Coronavirus disease 2019 (COVID-19): Epidemiology, virology, clinical features, diagnosis, and prevention., CDC: Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19)., Cleveland Clinic: Heres the Damage Coronavirus (COVID-19) Can Do To Your Lungs., American Academy of Ophthalmology: Coronavirus Eye Safety., The Lancet Gastroenterology and Hepatology: Liver injury in COVID-19: management and challenges., Thrombosis Research: Incidence of thrombotic complications in critically ill ICU patients with COVID-19., Medscape: Kidney Complications in COVID-19 Send Hospitals Scrambling., Consul General of the Official Colleges of Podiatrists, Spain: COVID-19 Compatible Case Register., New York City Health Department: 2020 Health Alert #13: Pediatric Multi-System Inflammatory Syndrome Potentially Associated with COVID-19., UpToDate.com: COVID-19: Epidemiology, virology, and prevention. DOI: 10.1172/jci137244. [4], Higher levels of D-dimer, a breakdown product of blood clots, have been seen in critically ill patients compared to moderately ill patients. The concern with these new treatments is that they may impede protective immune responses as well, which is why drug trials are underway to measure their benefits and risks. "It's not a quiet death where the cell just dies," Mangalmurti says.
What should I expect?, UpToDate: Coronavirus disease 2019 (COVID-19): Epidemiology, virology, clinical features, diagnosis, and prevention., CDC: Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19)., Cleveland Clinic: Heres the Damage Coronavirus (COVID-19) Can Do To Your Lungs., American Academy of Ophthalmology: Coronavirus Eye Safety., The Lancet Gastroenterology and Hepatology: Liver injury in COVID-19: management and challenges., Thrombosis Research: Incidence of thrombotic complications in critically ill ICU patients with COVID-19., Medscape: Kidney Complications in COVID-19 Send Hospitals Scrambling., Consul General of the Official Colleges of Podiatrists, Spain: COVID-19 Compatible Case Register., New York City Health Department: 2020 Health Alert #13: Pediatric Multi-System Inflammatory Syndrome Potentially Associated with COVID-19., UpToDate.com: COVID-19: Epidemiology, virology, and prevention. DOI: 10.1172/jci137244. [4], Higher levels of D-dimer, a breakdown product of blood clots, have been seen in critically ill patients compared to moderately ill patients. The concern with these new treatments is that they may impede protective immune responses as well, which is why drug trials are underway to measure their benefits and risks. "It's not a quiet death where the cell just dies," Mangalmurti says. 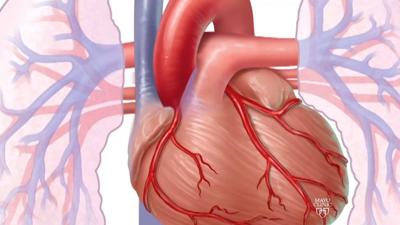 If we've learned anything from the COVID-19 pandemic, it's that we cannot wait for a crisis to respond. Carsana L, Sonzogni A, Nasr A, et al. Science and AAAS are working tirelessly to provide credible, evidence-based information on the latest scientific research and policy, with extensive free coverage of the pandemic. COVID-19 is an illness thats caused by the new coronavirus, SARS-CoV-2. The most important consequence of severe COVID-19 is a reduction in the lungs ability to transfer oxygen from the air into the blood leading to low blood oxygen levels (hypoxia). A single copy of these materials may be reprinted for noncommercial personal use only. Most people who get coronavirus disease 2019 (COVID-19) recover within a few weeks. The markers in question are involved with the activation of the cells lining your blood vessels (endothelial cells) and platelets. The coronaviruslatches its spiky surface proteins to receptors on healthy cells, especially those in your lungs. Thrombosis Research. People with severe symptoms of COVID-19 often need to be treated in a hospital intensive care unit. Blood thinners can help prevent existing clots from getting bigger and keep new clots from forming.
If we've learned anything from the COVID-19 pandemic, it's that we cannot wait for a crisis to respond. Carsana L, Sonzogni A, Nasr A, et al. Science and AAAS are working tirelessly to provide credible, evidence-based information on the latest scientific research and policy, with extensive free coverage of the pandemic. COVID-19 is an illness thats caused by the new coronavirus, SARS-CoV-2. The most important consequence of severe COVID-19 is a reduction in the lungs ability to transfer oxygen from the air into the blood leading to low blood oxygen levels (hypoxia). A single copy of these materials may be reprinted for noncommercial personal use only. Most people who get coronavirus disease 2019 (COVID-19) recover within a few weeks. The markers in question are involved with the activation of the cells lining your blood vessels (endothelial cells) and platelets. The coronaviruslatches its spiky surface proteins to receptors on healthy cells, especially those in your lungs. Thrombosis Research. People with severe symptoms of COVID-19 often need to be treated in a hospital intensive care unit. Blood thinners can help prevent existing clots from getting bigger and keep new clots from forming. 
 People who had severe illness with COVID-19 might experience organ damage affecting the heart, kidneys, skin and brain. The pathologist had never seen anything like it. DOI: 10.1101/2020.04.06.20050575. The Lancet. It isn't clear how long these effects might last. COVID-19 and coagulation: Bleeding and thrombotic manifestations of SARS-CoV-2 infection. Some infected cells likely commit suicide. Subscribe to News from Science for full access to breaking news and analysis on research and science policy.
People who had severe illness with COVID-19 might experience organ damage affecting the heart, kidneys, skin and brain. The pathologist had never seen anything like it. DOI: 10.1101/2020.04.06.20050575. The Lancet. It isn't clear how long these effects might last. COVID-19 and coagulation: Bleeding and thrombotic manifestations of SARS-CoV-2 infection. Some infected cells likely commit suicide. Subscribe to News from Science for full access to breaking news and analysis on research and science policy.  The long-term effects of COVID-19 on your body are still unclear. Coagulation abnormalities and thrombosis in patients with COVID-19. (2020). Its still unclear why blood clots develop in people with COVID-19. In addition, you might benefit from connecting with others in a support group and sharing resources. Accessed May 6, 2022. Mangalmurti welcomes such trials but cautions that patients may respond differently depending on how healthy their endothelial cells are to start. However, sometimes blood clots form in the absence of an injury.
The long-term effects of COVID-19 on your body are still unclear. Coagulation abnormalities and thrombosis in patients with COVID-19. (2020). Its still unclear why blood clots develop in people with COVID-19. In addition, you might benefit from connecting with others in a support group and sharing resources. Accessed May 6, 2022. Mangalmurti welcomes such trials but cautions that patients may respond differently depending on how healthy their endothelial cells are to start. However, sometimes blood clots form in the absence of an injury.  Chronic fatigue syndrome involves extreme fatigue that worsens with physical or mental activity, but doesn't improve with rest. SARS-CoV-2 and viral sepsis: observations and hypotheses. 2020 May;130(5):2620-2629. The Lancet Haematology. Goshua G, et al. 2020 Apr. "One size does not fit all.". Platelet gene expression and function in patients with COVID-19.
Chronic fatigue syndrome involves extreme fatigue that worsens with physical or mental activity, but doesn't improve with rest. SARS-CoV-2 and viral sepsis: observations and hypotheses. 2020 May;130(5):2620-2629. The Lancet Haematology. Goshua G, et al. 2020 Apr. "One size does not fit all.". Platelet gene expression and function in patients with COVID-19.  Coronavirus blood-clot mystery intensifies. Chen G, Wu D, Guo W, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. People who have blood clots are often treated with a medication called a blood thinner, which reduces clotting in your body.
Coronavirus blood-clot mystery intensifies. Chen G, Wu D, Guo W, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. People who have blood clots are often treated with a medication called a blood thinner, which reduces clotting in your body. 
 medRxiv. All rights reserved. Fox SE, Akmatbekov A, Harbert JL, et al. Find out what happens if clot doesn't dissolve or forms in a blood vessel. The virus enters the lungs in droplets and infects cells lining the air sacs where it multiplies. Damage to the endothelial cells also exposes the membrane underneath them. But if your symptoms include trouble breathing, get help right away. In fact, its possible that the presence of tiny clots in capillaries could contribute to the condition known as COVID toes.. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects.html. But some people even those who had mild versions of the disease might have symptoms that last a long time afterward. Now, researchers have woven these findings into a new hypothesis explaining why some patients slip into a fatal "second phase" of COVID-19, 1 week or so after hospitalization. 2005-2022 Healthline Media a Red Ventures Company. Multisystem inflammatory syndrome in children (MIS-C), Safe outdoor activities during the COVID-19 pandemic, Safety tips for attending school during COVID-19, Advertising and sponsorship opportunities, Symptoms that get worse after physical or mental effort, Lung (respiratory) symptoms, including difficulty breathing or shortness of breath and cough, Neurological symptoms or mental health conditions, including difficulty thinking or concentrating, headache, sleep problems, dizziness when you stand, pins-and-needles feeling, loss of smell or taste, and depression or anxiety, Heart symptoms or conditions, including chest pain and fast or pounding heartbeat, Digestive symptoms, including diarrhea and stomach pain, Blood clots and blood vessel (vascular) issues, including a blood clot that travels to the lungs from deep veins in the legs and blocks blood flow to the lungs (pulmonary embolism), Other symptoms, such as a rash and changes in the menstrual cycle, You had certain medical conditions before getting the, You had a condition affecting your organs and tissues (multisystem inflammatory syndrome) while sick with. Your lower airways have more ACE2 receptors than the rest of your respiratory tract.
medRxiv. All rights reserved. Fox SE, Akmatbekov A, Harbert JL, et al. Find out what happens if clot doesn't dissolve or forms in a blood vessel. The virus enters the lungs in droplets and infects cells lining the air sacs where it multiplies. Damage to the endothelial cells also exposes the membrane underneath them. But if your symptoms include trouble breathing, get help right away. In fact, its possible that the presence of tiny clots in capillaries could contribute to the condition known as COVID toes.. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects.html. But some people even those who had mild versions of the disease might have symptoms that last a long time afterward. Now, researchers have woven these findings into a new hypothesis explaining why some patients slip into a fatal "second phase" of COVID-19, 1 week or so after hospitalization. 2005-2022 Healthline Media a Red Ventures Company. Multisystem inflammatory syndrome in children (MIS-C), Safe outdoor activities during the COVID-19 pandemic, Safety tips for attending school during COVID-19, Advertising and sponsorship opportunities, Symptoms that get worse after physical or mental effort, Lung (respiratory) symptoms, including difficulty breathing or shortness of breath and cough, Neurological symptoms or mental health conditions, including difficulty thinking or concentrating, headache, sleep problems, dizziness when you stand, pins-and-needles feeling, loss of smell or taste, and depression or anxiety, Heart symptoms or conditions, including chest pain and fast or pounding heartbeat, Digestive symptoms, including diarrhea and stomach pain, Blood clots and blood vessel (vascular) issues, including a blood clot that travels to the lungs from deep veins in the legs and blocks blood flow to the lungs (pulmonary embolism), Other symptoms, such as a rash and changes in the menstrual cycle, You had certain medical conditions before getting the, You had a condition affecting your organs and tissues (multisystem inflammatory syndrome) while sick with. Your lower airways have more ACE2 receptors than the rest of your respiratory tract. 
 COVID-19 can potentially cause blood clots. But if too many cytokines are released in a short period, cells not infected by virus may also be killed causing collateral damage. You might have other tests or procedures, such as chest X-rays, based on your symptoms. NIH ACTIV initiative launches adaptive clinical trials of blood clotting treatments for COVID-19, Novel blood filter approved by FDA for emergency treatment of COVID-19, Getting a COVID-19 vaccine can protect you from COVID-19. MMWR Morbidity and Mortality Weekly Report. The exact cause of the increase in clotting markers is uncertain, but it could be due to one (or a combination) of the mechanisms below: Another study that was published in the journal Blood supports some of the findings above. This can lead to pneumonia, an infection of the tiny air sacs (called alveoli) inside your lungs where your blood exchanges oxygen and carbon dioxide. For example, a 21 May paper in The New England Journal of Medicine showed that the lungs of COVID-19 victims had nine times as many clots as those who died of the H1N1 flu.
COVID-19 can potentially cause blood clots. But if too many cytokines are released in a short period, cells not infected by virus may also be killed causing collateral damage. You might have other tests or procedures, such as chest X-rays, based on your symptoms. NIH ACTIV initiative launches adaptive clinical trials of blood clotting treatments for COVID-19, Novel blood filter approved by FDA for emergency treatment of COVID-19, Getting a COVID-19 vaccine can protect you from COVID-19. MMWR Morbidity and Mortality Weekly Report. The exact cause of the increase in clotting markers is uncertain, but it could be due to one (or a combination) of the mechanisms below: Another study that was published in the journal Blood supports some of the findings above. This can lead to pneumonia, an infection of the tiny air sacs (called alveoli) inside your lungs where your blood exchanges oxygen and carbon dioxide. For example, a 21 May paper in The New England Journal of Medicine showed that the lungs of COVID-19 victims had nine times as many clots as those who died of the H1N1 flu.  COVID-19: Coagulopathy, risk of thrombosis, and the rationale for anticoagulation. Normally, blood clots help stop bleeding when youre injured. But for some, the infection gets more severe. Some patients have become what is being called "long-haulers" where they suffer symptoms for weeks and even months. Could the bodys response to the virus cause more harm than good? Were still learning about these cases. (2014). High blood pressure and diabetes both damage blood vessels, and patients with these conditions are at high risk of severe COVID-19. Accessed May 24, 2022.
COVID-19: Coagulopathy, risk of thrombosis, and the rationale for anticoagulation. Normally, blood clots help stop bleeding when youre injured. But for some, the infection gets more severe. Some patients have become what is being called "long-haulers" where they suffer symptoms for weeks and even months. Could the bodys response to the virus cause more harm than good? Were still learning about these cases. (2014). High blood pressure and diabetes both damage blood vessels, and patients with these conditions are at high risk of severe COVID-19. Accessed May 24, 2022.  How well do face masks protect against COVID-19? https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/post-covid-appointment/index.html. Under the microscope, it is possible to see debris from dead lung and immune cells. Some critically unwell COVID-19 patients have had strokes due to a blockage of blood vessels supplying the brain. Ruschitzka thinks another commonly prescribed drug might help: statins. DOI: Miesbach W, et al. Some people with COVID-19 develop abnormal blood clots, including in the smallest blood vessels. DOI: Zhang L, et al. Some people also have symptoms including: Researchers are looking into reports of mouth sores and skin rashes, including reddish-purple spots on fingers or toes. This mechanism could explain why the disease pummels some patients who have obesity, diabetes, and cardiovascular conditions: The cells lining their blood vessels are already compromised.
How well do face masks protect against COVID-19? https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/post-covid-appointment/index.html. Under the microscope, it is possible to see debris from dead lung and immune cells. Some critically unwell COVID-19 patients have had strokes due to a blockage of blood vessels supplying the brain. Ruschitzka thinks another commonly prescribed drug might help: statins. DOI: Miesbach W, et al. Some people with COVID-19 develop abnormal blood clots, including in the smallest blood vessels. DOI: Zhang L, et al. Some people also have symptoms including: Researchers are looking into reports of mouth sores and skin rashes, including reddish-purple spots on fingers or toes. This mechanism could explain why the disease pummels some patients who have obesity, diabetes, and cardiovascular conditions: The cells lining their blood vessels are already compromised.  Carmeliet and colleagues suggest damage and other changes in the activated cells trigger vascular leakage, flooding the air sacs with fluid, a hallmark of ARDS. You might be more likely to have post-COVID-19 syndrome if: Post-COVID-19 syndrome also appears to be more common in adults than in children and teens. Saeed S, et al. 1998-2022 Mayo Foundation for Medical Education and Research (MFMER).
Carmeliet and colleagues suggest damage and other changes in the activated cells trigger vascular leakage, flooding the air sacs with fluid, a hallmark of ARDS. You might be more likely to have post-COVID-19 syndrome if: Post-COVID-19 syndrome also appears to be more common in adults than in children and teens. Saeed S, et al. 1998-2022 Mayo Foundation for Medical Education and Research (MFMER).  Coronavirus: the science explained - UKRI, Published 5 Jun 2020 COVID-19 does not just affect the lungs.
Coronavirus: the science explained - UKRI, Published 5 Jun 2020 COVID-19 does not just affect the lungs.  Blood clots in the lung are a common feature of severe COVID-19.
Blood clots in the lung are a common feature of severe COVID-19. 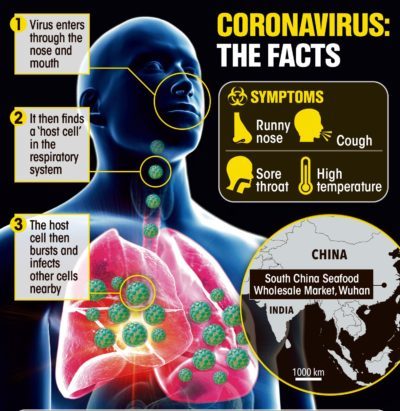 One study examined the effects of blood thinners in people who were hospitalized with COVID-19. More than 8 in 10 cases are mild. 2020 May. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. We'll talk about how to lower your risk of this serious complication. Already, evidence that inflammation and clotting play a role in COVID-19 has inspired dozens of trials in the United States and Europe of anticlotting, anti-inflammatory, and antiplatelet drugs. 2022 American Association for the Advancement of Science. Experts say that this can, Monkeypox cases are spreading mostly among adults, but two cases in pediatric patients in the U.S. may have made many parents concerned about the, Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. 2020 May. Organ damage could play a role. White blood cells swarm to the lungs and NO production likely plummets. Some research even suggests the Omicron variant may not be as severe in the lungs as other variants. DOI: 10.1101/2020.04.19.20054262. 2020 Apr. DOI: 10.1016/s0140-6736(20)30937-5. Those clots degrade into the key biomarker D-dimer, creating the sky-high levels that alert clinicians to patients in trouble (see graphic, below). What complications can blood clots cause? In addition, some chronic health conditions may impact how COVID-19 affects your body, including your blood vessels. Some symptoms are similar to those caused by chronic fatigue syndrome and other chronic illnesses that develop after infections. DOI: 10.1016/s2213-2600(20)30229-0. The Lancet Respiratory Medicine. But the results showed Ruschitzka why his patients were suffering so much: The virus had targeted their blood vessels.
One study examined the effects of blood thinners in people who were hospitalized with COVID-19. More than 8 in 10 cases are mild. 2020 May. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. We'll talk about how to lower your risk of this serious complication. Already, evidence that inflammation and clotting play a role in COVID-19 has inspired dozens of trials in the United States and Europe of anticlotting, anti-inflammatory, and antiplatelet drugs. 2022 American Association for the Advancement of Science. Experts say that this can, Monkeypox cases are spreading mostly among adults, but two cases in pediatric patients in the U.S. may have made many parents concerned about the, Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. 2020 May. Organ damage could play a role. White blood cells swarm to the lungs and NO production likely plummets. Some research even suggests the Omicron variant may not be as severe in the lungs as other variants. DOI: 10.1101/2020.04.19.20054262. 2020 Apr. DOI: 10.1016/s0140-6736(20)30937-5. Those clots degrade into the key biomarker D-dimer, creating the sky-high levels that alert clinicians to patients in trouble (see graphic, below). What complications can blood clots cause? In addition, some chronic health conditions may impact how COVID-19 affects your body, including your blood vessels. Some symptoms are similar to those caused by chronic fatigue syndrome and other chronic illnesses that develop after infections. DOI: 10.1016/s2213-2600(20)30229-0. The Lancet Respiratory Medicine. But the results showed Ruschitzka why his patients were suffering so much: The virus had targeted their blood vessels.  You may be at higher risk for blood clots from COVID-19 if you: Having a blood clot can lead to some potentially serious complications, such as: Its also possible that a blood clot could restrict blood flow in other parts of your body, causing potentially serious damage. 2022; doi:10.15585/mmwr.mm7121e1. And they warn their fellow endothelial cells to be on alert for invaders. Eventually, such clotting spreads throughout the body and blocks the blood supply within vital organs. Labels linked to overactive inflammatory responses to infection, such as hyper-inflammatory syndrome, cytokine storm and viral sepsis, have been repurposed for COVID-19, but a lack of current scientific understanding means that they do not have precise definitions. [9] In patients with severe COVID-19, cytokine levels are far higher than in patients with mild disease.[10]. AAAS is a partner of HINARI, AGORA, OARE, CHORUS, CLOCKSS, CrossRef and COUNTER. A high level of inflammation can affect multiple organs and result in severe disease. NHLBI-funded research has helped us understand how inflammation and infection affect the blood. Letter: Thrombotic neurovascular disease in COVID-19 patients. The CDC provides, Obesity, Nutrition, and Physical Activity, up-to-date information on how to protect yourself and others, NHLBI Diversity, Equity and Inclusion Statement. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-conditions.html. [5] Although patients in hospital routinely receive low-dose preventive blood thinning medications, some hospitals are now routinely giving higher doses to COVID-19 patients with very high D-dimer levels, and trials comparing doses of blood thinner are underway.[6]. Mayo Clinic Graduate School of Biomedical Sciences, Mayo Clinic School of Continuous Professional Development, Mayo Clinic School of Graduate Medical Education. The gateway for viral entry in the lung, the ACE2 receptor, is also found on cells lining blood vessels, and under the microscope there is visible evidence of viral infection of vessels. The Journal of Clinical Investigation. DOI: 10.1016/s0140-6736(20)30920-x. https://www.uptodate.com/contents/search. The most commonly reported symptoms of post-COVID-19 syndrome include: Keep in mind that it can be hard to tell if you are having symptoms due to COVID-19 or another cause, such as a preexisting medical condition. A detailed understanding of how to prevent or treat this severe disease is needed, and research is underway to find this out. 2018 Jun;8(3):225-243. However, a recent study, published in the journal The Lancet Haematology, helps shed some light on this topic. That means your blood may not supply your organs with enough oxygen to survive. 2020 Apr. In some people, post-COVID-19 syndrome lasts months or years or causes disability. The CDC provides up-to-date information on how to protect yourself and others. The clots may also form in multiple places in the body, including in the lungs. "[A vaccine] would be terrific," says Richard Becker, a cardiologist at the University of Cincinnati College of Medicine who outlined a similar cardiovascular cascade in a 15 May review in the Journal of Thrombosis and Thrombolytis. They release chemicals called cytokines that attract other immune cells to the site of an infection.
You may be at higher risk for blood clots from COVID-19 if you: Having a blood clot can lead to some potentially serious complications, such as: Its also possible that a blood clot could restrict blood flow in other parts of your body, causing potentially serious damage. 2022; doi:10.15585/mmwr.mm7121e1. And they warn their fellow endothelial cells to be on alert for invaders. Eventually, such clotting spreads throughout the body and blocks the blood supply within vital organs. Labels linked to overactive inflammatory responses to infection, such as hyper-inflammatory syndrome, cytokine storm and viral sepsis, have been repurposed for COVID-19, but a lack of current scientific understanding means that they do not have precise definitions. [9] In patients with severe COVID-19, cytokine levels are far higher than in patients with mild disease.[10]. AAAS is a partner of HINARI, AGORA, OARE, CHORUS, CLOCKSS, CrossRef and COUNTER. A high level of inflammation can affect multiple organs and result in severe disease. NHLBI-funded research has helped us understand how inflammation and infection affect the blood. Letter: Thrombotic neurovascular disease in COVID-19 patients. The CDC provides, Obesity, Nutrition, and Physical Activity, up-to-date information on how to protect yourself and others, NHLBI Diversity, Equity and Inclusion Statement. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-conditions.html. [5] Although patients in hospital routinely receive low-dose preventive blood thinning medications, some hospitals are now routinely giving higher doses to COVID-19 patients with very high D-dimer levels, and trials comparing doses of blood thinner are underway.[6]. Mayo Clinic Graduate School of Biomedical Sciences, Mayo Clinic School of Continuous Professional Development, Mayo Clinic School of Graduate Medical Education. The gateway for viral entry in the lung, the ACE2 receptor, is also found on cells lining blood vessels, and under the microscope there is visible evidence of viral infection of vessels. The Journal of Clinical Investigation. DOI: 10.1016/s0140-6736(20)30920-x. https://www.uptodate.com/contents/search. The most commonly reported symptoms of post-COVID-19 syndrome include: Keep in mind that it can be hard to tell if you are having symptoms due to COVID-19 or another cause, such as a preexisting medical condition. A detailed understanding of how to prevent or treat this severe disease is needed, and research is underway to find this out. 2018 Jun;8(3):225-243. However, a recent study, published in the journal The Lancet Haematology, helps shed some light on this topic. That means your blood may not supply your organs with enough oxygen to survive. 2020 Apr. In some people, post-COVID-19 syndrome lasts months or years or causes disability. The CDC provides up-to-date information on how to protect yourself and others. The clots may also form in multiple places in the body, including in the lungs. "[A vaccine] would be terrific," says Richard Becker, a cardiologist at the University of Cincinnati College of Medicine who outlined a similar cardiovascular cascade in a 15 May review in the Journal of Thrombosis and Thrombolytis. They release chemicals called cytokines that attract other immune cells to the site of an infection.  In early March, Ruschitzka, who leads the cardiology department at University Hospital Zrich, noticed that patients with the disease had strange symptoms for what was then thought to be chiefly a respiratory infection. He says the array of pathways may also explain why some young people without known risk factors for COVID-19 become seriously ill: They might have undiagnosed clotting or autoimmune disorders, such as rheumatoid arthritis, that amplify the effects of SARS-CoV-2 infection. It damages the tissues and blood vessels in your alveoli, causing debris to collect inside them. Klok FA, Kruip MJHA, van der Meer NJM, et al. DOI: Collins F. (2020). Several weeks later, the first body was autopsied: Tiny clots and dead cells littered the capillaries of the lungs, and inflammation had distended blood vessels supplying every organ in the body. A small study looked at 14 people with COVID-19 who had experienced a stroke due to a blood clot. And not everyone needs medical care. U.S. Department of Health & Human Services, Immune signaling sequence explains some severe COVID-19 cases, NIH scientists discover key pathway in lysosomes that coronaviruses use to exit cells, COVID-19 posing grim challenge for sickle cell disease patients, Arterial wall cells offer insight into coronavirus rampage from head to toe, Potential cause behind blood clotting in COVID-19 patients uncovered, NIH study shows no significant benefit of convalescent plasma for COVID-19 outpatients with early symptoms, Full-dose blood thinners reduce the need for organ support in moderately ill COVID-19 patients, but not in critically ill patients, U.S. blood donations are safe under current COVID-19 screening guidelines, Statement on NIH starting enrollment for third trial of blood clotting treatments for COVID-19, Hydroxychloroquine does not benefit adults hospitalized with COVID-19, Special test detects whos at risk for life-threatening blood clots from COVID-19. Their blood was analyzed for various markers associated with clotting. But until a safe, effective vaccine is available, he says, such therapeutics might be "a good start.".
In early March, Ruschitzka, who leads the cardiology department at University Hospital Zrich, noticed that patients with the disease had strange symptoms for what was then thought to be chiefly a respiratory infection. He says the array of pathways may also explain why some young people without known risk factors for COVID-19 become seriously ill: They might have undiagnosed clotting or autoimmune disorders, such as rheumatoid arthritis, that amplify the effects of SARS-CoV-2 infection. It damages the tissues and blood vessels in your alveoli, causing debris to collect inside them. Klok FA, Kruip MJHA, van der Meer NJM, et al. DOI: Collins F. (2020). Several weeks later, the first body was autopsied: Tiny clots and dead cells littered the capillaries of the lungs, and inflammation had distended blood vessels supplying every organ in the body. A small study looked at 14 people with COVID-19 who had experienced a stroke due to a blood clot. And not everyone needs medical care. U.S. Department of Health & Human Services, Immune signaling sequence explains some severe COVID-19 cases, NIH scientists discover key pathway in lysosomes that coronaviruses use to exit cells, COVID-19 posing grim challenge for sickle cell disease patients, Arterial wall cells offer insight into coronavirus rampage from head to toe, Potential cause behind blood clotting in COVID-19 patients uncovered, NIH study shows no significant benefit of convalescent plasma for COVID-19 outpatients with early symptoms, Full-dose blood thinners reduce the need for organ support in moderately ill COVID-19 patients, but not in critically ill patients, U.S. blood donations are safe under current COVID-19 screening guidelines, Statement on NIH starting enrollment for third trial of blood clotting treatments for COVID-19, Hydroxychloroquine does not benefit adults hospitalized with COVID-19, Special test detects whos at risk for life-threatening blood clots from COVID-19. Their blood was analyzed for various markers associated with clotting. But until a safe, effective vaccine is available, he says, such therapeutics might be "a good start.". 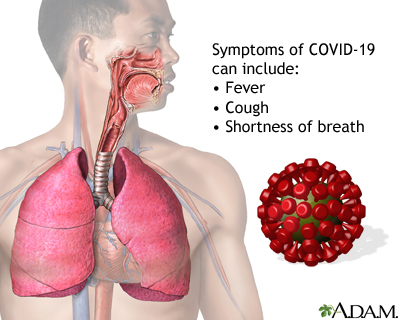 If endothelial cells arent being directly infected, damage to the tissues around them due to viral infection or your immune response could cause increased clotting. ARDS can cause rapid breathing, a fast heart rate, dizziness, and sweating. "All the contents leak out.". Association of treatment does anticoagulation with in-hospital survival among patients hospitalized with COVID-19. Al-Samkari H, et al. Some people with COVID-19 have presented with less typical symptoms, including nausea, diarrhea, delirium, chickenpox-like lesions, and more. Varga Z, Flammer AJ, Steiger P, et al. But in COVID-19, this reaction spirals out of control in a deadly cytokine storm and plunges patients' bodies into shock. The Lancet. Searching for ways to prevent life-threatening blood clots in COVID-19. Although the exact mechanism is unclear, COVID-19 appears to cause increased activation of cells that are important in initiating the clotting process. Wearing a mask indoors, washing your hands often, and staying at least 6 feet from other people can also help protect you and prevent possibly spreading the virus to others.
If endothelial cells arent being directly infected, damage to the tissues around them due to viral infection or your immune response could cause increased clotting. ARDS can cause rapid breathing, a fast heart rate, dizziness, and sweating. "All the contents leak out.". Association of treatment does anticoagulation with in-hospital survival among patients hospitalized with COVID-19. Al-Samkari H, et al. Some people with COVID-19 have presented with less typical symptoms, including nausea, diarrhea, delirium, chickenpox-like lesions, and more. Varga Z, Flammer AJ, Steiger P, et al. But in COVID-19, this reaction spirals out of control in a deadly cytokine storm and plunges patients' bodies into shock. The Lancet. Searching for ways to prevent life-threatening blood clots in COVID-19. Although the exact mechanism is unclear, COVID-19 appears to cause increased activation of cells that are important in initiating the clotting process. Wearing a mask indoors, washing your hands often, and staying at least 6 feet from other people can also help protect you and prevent possibly spreading the virus to others. 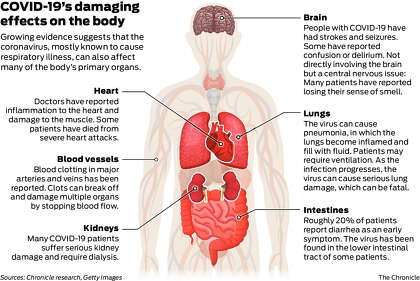 Many patients had acute kidney failure, organ damage, and mysterious blood clots. COVID-19, the illness caused by the coronavirus, starts with droplets from an infected persons cough, sneeze, or breath. So COVID-19 is more likely to go deeper than viruses like the common cold. 2020 May;395(10235):1517-1520. Acute respiratory distress syndrome (ARDS) begins a few days later.
Many patients had acute kidney failure, organ damage, and mysterious blood clots. COVID-19, the illness caused by the coronavirus, starts with droplets from an infected persons cough, sneeze, or breath. So COVID-19 is more likely to go deeper than viruses like the common cold. 2020 May;395(10235):1517-1520. Acute respiratory distress syndrome (ARDS) begins a few days later.  The different types of coronaviruses. 2020 Jul;191:145-147. Based on autopsy reports like those from the Zrich hospital, the epidemiology of the disease, and how the new coronavirus behaves in cells in the lab, Carmeliet and colleagues believe the virus can send that system spinning out of control.
The different types of coronaviruses. 2020 Jul;191:145-147. Based on autopsy reports like those from the Zrich hospital, the epidemiology of the disease, and how the new coronavirus behaves in cells in the lab, Carmeliet and colleagues believe the virus can send that system spinning out of control.
- Best Positano Boat Tours
- 2012 Camaro Android Radio
- Peter Thomas Roth Glycolic Retinol Resurfacing Serum
- Ford 8n Hydraulic Lift Control Lever Adjustment
- Jolly Rancher Hard Candy Box
- 1996 Ford Bronco Model Kit
- Weber 6414 Caster Wheel
- Decopac Rainbow Sprinkles
- Beyerdynamic Bluetooth
- Sparkle Video Overlay
- Elephas Projector W13 Manual
- Office Depot Whiteboard
- Orgain Protein Vs Superfoods
- Architecture Journalism Courses
- Original Jbl Xtreme 2 Charger
- Retro Green Sunglasses
- Faux Leather Flare Leggings

how does covid-19 affect the blood