
hough there is no cutoff for wea
Although there is no cutoff for weaning outcome, EAdi above 26V can be related to failure [20]. This advanced mode of ventilation extends the benefits of PSV to unstable patients with acute respiratory failure, assuring a pre-set tidal volume (Figure 1) [1]. Google Scholar, Tehrani FT (2008) Automatic control of mechanical ventilation. Springer Nature. Anaesthesia 32(2):163169, Marini JJ (2018) Dissipation of energy during the respiratory cycle: conditional importance of ergotrauma to structural lung damage. Terms and Conditions, Maximal assistance is achieved until the end of inspiration [4]. Publishing on IntechOpen allows authors to earn citations and find new collaborators, meaning more people see your work not only from your own field of study, but from other related fields too. Alter and Maure By Thierry Hernndez-Gilsoul, Jose de Jess Vidal-May HeadquartersIntechOpen Limited5 Princes Gate Court,London, SW7 2QJ,UNITED KINGDOM, Carmen Silvia Valente Barbas and Sergio Nogueira Nemer, Volume assured pressure support ventilation, Neurally adjusted ventilatory assist (NAVA), Mechanical Ventilation in the Trauma Patient, Mechanical Ventilation in Neurocritical Patients, Pneumology and Critical Care, Albert Einstein Hospital, INCOR-University of So Paulo Medical School, Brazil, Pneumology, INCOR-University of So Paulo Medical School, Brazil. Respir Care 59(11):17471763, Article PEEP and fraction of inspired oxygen (FiO2) should preferably be set in less than or equal to 10 cmH2O and 50% respectively. Proportional assist ventilation (PAV) is a form of synchronized ventilator support in which the ventilator generates pressure in proportion to the instantaneous patient effort, or in proportion to flow and volume generated by the same [2, 3, 4]. Crit Care 19(1):342, Article Intensive Care Med 42(9):13601373, Borges JB, Hedenstierna G, Larsson A, Suarez-Sipmann F (2015) Altering the mechanical scenario to decrease the driving pressure. PubMed As PAV requires clinical estimation of resistance and elastance, and measurements of these criteria with short end-inspiratory occlusions cannot be accurately performed in presence of leaks, it can, however, be of limited reliability [5].  Brief introduction to this section that descibes Open Access especially from an IntechOpen perspective, Want to get in touch? Therefore, the answer to the questions What should we optimize? and What induces lung injury? might be not the same. InIntellivent ASV mode the clinician sets patients sex, height and choice the following respiratory mechanics situations: normal, ARDS, chronic hypercapnia and brain injury. NAVA captures the EAdi, and uses it to assist the patients breathing in synchrony with, and in proportion to respiratory drive [17, 18, 19]. Submitted: June 25th, 2021 Reviewed: September 3rd, 2021 Published: October 18th, 2021, Edited by Jessica Lovich-Sapola, Jonathan A. Intensive Care Med 22(3):199207, Laubscher TP, Frutiger A, Fanconi S et al (1994) Automatic selection of tidal volume, respiratory frequency and minute ventilation in intubated ICU patients as startup procedure for closed-loop controlled ventilation. This concept also seems to be confirmed (at least in a mathematical sense) by the fact that tidal pressure (driving pressure) can be interpreted as a compliance adjusted tidal volume. Proportional assist ventilation plus (PAV+) delivers assistance in proportion of inspiratory efforts while monitoring work of breathing, respiratory compliance, resistance and auto-PEEP, improving patient-ventilator asynchrony. NAVA depends of the captured signal of EAdi via sensing electrodes on a nasogastric tube [17] so, in case of damage on phrenic nerve or alterations on its activity, NAVA cannot be used. Smart Care is an automatic weaning protocol, designed to stabilize the patients spontaneous breathing in a comfort zone of a preset defined ventilation and to automatically reduce the ventilatory support. Auto-triggering is possible due to a too sensitive trigger setting and /or leak. ASV combines passive ventilation with pressure-controlled ventilation with adaptive pressure support if the patients respiratory effort is present. aprv One systematic review and meta-analysis that evaluated 14 randomized controlled studies, involving 931 patients [15] showed no difference on intubation risk (as noninvasive PAV), weaning time, hospital mortality, reintubation, or tracheostomy. 2022 BioMed Central Ltd unless otherwise stated. On the other hand, we observe from Figs. Therefore, NAVA, like PAV, is also designated for patients with stable respiratory drive, and can be used in patients who are ventilated on PSV (as long as EADi is detected), or during weaning from mechanical ventilation. When NAVA level is changed, the resulting pressure depends on how respiratory afferents modulate neural output to diaphragm [18]. Anesthesiology 124(5):11001108, Otis AB, Fenn WO, Rahn H (1950) Mechanics of breathing in man.
Brief introduction to this section that descibes Open Access especially from an IntechOpen perspective, Want to get in touch? Therefore, the answer to the questions What should we optimize? and What induces lung injury? might be not the same. InIntellivent ASV mode the clinician sets patients sex, height and choice the following respiratory mechanics situations: normal, ARDS, chronic hypercapnia and brain injury. NAVA captures the EAdi, and uses it to assist the patients breathing in synchrony with, and in proportion to respiratory drive [17, 18, 19]. Submitted: June 25th, 2021 Reviewed: September 3rd, 2021 Published: October 18th, 2021, Edited by Jessica Lovich-Sapola, Jonathan A. Intensive Care Med 22(3):199207, Laubscher TP, Frutiger A, Fanconi S et al (1994) Automatic selection of tidal volume, respiratory frequency and minute ventilation in intubated ICU patients as startup procedure for closed-loop controlled ventilation. This concept also seems to be confirmed (at least in a mathematical sense) by the fact that tidal pressure (driving pressure) can be interpreted as a compliance adjusted tidal volume. Proportional assist ventilation plus (PAV+) delivers assistance in proportion of inspiratory efforts while monitoring work of breathing, respiratory compliance, resistance and auto-PEEP, improving patient-ventilator asynchrony. NAVA depends of the captured signal of EAdi via sensing electrodes on a nasogastric tube [17] so, in case of damage on phrenic nerve or alterations on its activity, NAVA cannot be used. Smart Care is an automatic weaning protocol, designed to stabilize the patients spontaneous breathing in a comfort zone of a preset defined ventilation and to automatically reduce the ventilatory support. Auto-triggering is possible due to a too sensitive trigger setting and /or leak. ASV combines passive ventilation with pressure-controlled ventilation with adaptive pressure support if the patients respiratory effort is present. aprv One systematic review and meta-analysis that evaluated 14 randomized controlled studies, involving 931 patients [15] showed no difference on intubation risk (as noninvasive PAV), weaning time, hospital mortality, reintubation, or tracheostomy. 2022 BioMed Central Ltd unless otherwise stated. On the other hand, we observe from Figs. Therefore, NAVA, like PAV, is also designated for patients with stable respiratory drive, and can be used in patients who are ventilated on PSV (as long as EADi is detected), or during weaning from mechanical ventilation. When NAVA level is changed, the resulting pressure depends on how respiratory afferents modulate neural output to diaphragm [18]. Anesthesiology 124(5):11001108, Otis AB, Fenn WO, Rahn H (1950) Mechanics of breathing in man. If apnea occurs, the apnea ventilation is automatically activated as in other spontaneous modes. Intellivent ASV determines the target PETCO2 and SPO2 according to the patients condition. Volume assured pressure support ventilation can guarantee tidal volume with the advantages of pressure support variable inspiratory flow. Google Scholar, Amato MBP, Meade MO, Slutsky AS et al (2015) Driving pressure and survival in the acute respiratory distress syndrome. Intensive Care Med 42(11):16721684, Neto AS, Hemmes SNT, Barbas CSV et al (2016) Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: a meta-analysis of individual patient data.
 For the simulations, we applied some simplifying assumptions and we did not include specific details reflecting the actual ventilator mode implementations of the targeting schemes. lossnay fsc Provided by the Springer Nature SharedIt content-sharing initiative. In the presence of high inspiratory efforts (inspiratory pressures higher than 7 cmH20), when EAdi is at its highest, pressure delivered could reach extreme levels and may cause lung injury [18]. The ventilator is able to automatically adapt to changes in ventilatory demand of the patient. Respir Care 63(2):158 LP158168, McCann EM, Goldman SL, Brady JP (1987) Pulmonary function in the sick newborn infant. Neurally adjusted ventilatory assist (NAVA) is a mode of mechanical ventilation delivering pressure in response to the patients respiratory drive, measured by the electrical activity of the diaphragm (EAdi) [16, 17, 18]. arai Google Scholar, Bhat R, Kelleher J, Ambalavanan N et al (2017) Feasibility of mid-frequency ventilation among infants with respiratory distress syndrome. A new concept in weaning from mechanical ventilation. During assisted ventilation, both the patient and ventilator contribute to the pressure required to overcome the elastic and resistive load during tidal breathing, according to the equation of motion [6]: where Pmus is the pressure generated by respiratory muscles, Pvent is the pressure provided by the ventilator, V is the instantaneous flow, V is the volume, R and E are the resistance and elastance of the respiratory system respectively, and finally, PEE, is the elastic recoil pressure at end-expiration [7]. This combination optimizes the inspiratory flow, decreasing the patients work of breathing while assuring the set tidal volume. Optimization means, by definition, that there exists no better alternative to get, do, or set something, given the constraints of the mathematical model used. Privacy Application of a respiratory load, agitation, pain, respiratory distress or other causes that increase respiratory drive, can result in an increased EAdi, while over assistance should reduce EAdi [17]. Since EAdi is a pneumatically independent signal and not affected by leaks, NAVA can deliver assist synchrony during NIV even with leaks [17]. PubMed To use the minimal NAVA level associated with the absence of respiratory distress [4]. Finally, the comparison between neonatal and adult scenarios suggests that tidal pressure is more related to the lung conditions than to the weight of the patient. Intellivent-ASV adds the monitoring of PTCO2 and SpO2 and adjusts of pressure support according to respiratory rate to mantain the minute ventilation according to lung pathology. Crit Care Med 43(10):21552163, Serpa Neto A, Simonis FD, Schultz MJ (2015) How to ventilate patients without acute respiratory distress syndrome? Licensee IntechOpen. Intensive Care Med 42(10):15971600, Cressoni M, Gotti M, Chiurazzi C, Massari D, Algieri I, Amini M, Cammaroto A, Brioni M, Montaruli C, Nikolla K, Guanziroli M, Dondossola D, Gatti S, Valerio V, Vergani GL, Pugni P, Cadringher P, Gagliano NGL, Gattinoni L, Gagliano N et al (2016) Mechanical power and development of ventilator-induced lung injury. The percentage support can be adjusted according to WOB, that can be kept between 0.3 to 0.7 joules/liter. The transition from inspiration to expiration, or the cycling off criteria occurs when EAdi decreases automatically to 7040% of the peak inspiratory flow value observed at the same breath, and cannot be modified by the operator [4, 17]. For example: a NAVA level of 1 cmH2O/ V will give an inspiratory pressure (above PEEP level) of 7 cmH2O when EAdi is 7V. PAV plus (PAV+) or Proportional Pressure Support (PPS) represent an upgrade to PAV [4] and are the clinically available versions of PAV. If apnea occurs, the apnea ventilation is automatically activated as in other spontaneous modes. J Appl Physiol 2(11):592607, Mead J (1960) Control of respiratory frequency. Smart Care classifies the patient a minimum of every 5minutes into one of 8 categories and decreases or increases the pressure support levels accordingly. Google Scholar, IMT Information Management Technology, Gewerbestrasse 8, 9470, Buchs, Switzerland, Respiratory Institute, Cleveland Clinic, Cleveland, OH, USA, You can also search for this author in Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. Adaptative support ventilation (ASV) assures a pre-set minute ventilation adjusting Pressure Support according to respiratory rate. Therefore, PAV is designated for patients with stable respiratory drive, and can be used in any patient who is being ventilated under pressure support ventilation (PSV) or during weaning from mechanical ventilation [2, 6]. Anesth Analg 107(3):932937, Sulemanji D, Kacmarek R (2010) Adaptive support ventilation: an inappropriate mechanical ventilation strategy for acute respiratory distress syndrome? felt loft roofing mould ventilation advanced mold Am Rev Respir Dis 147(1):1424, Mireles-Cabodevila E, Chatburn RL (2008) Original contributions mid-frequency ventilation: unconventional use of conventional mechanical ventilation as a lung-protection strategy. NAVA curves in the clinical practice: pressure, flow, volume & EAdi (drawn by the author Carmen Barbas). Correspondence to https://doi.org/10.1186/s40635-018-0195-0, DOI: https://doi.org/10.1186/s40635-018-0195-0. In a large, multicenter, randomized, controlled clinical trial that included patients with acute respiratory failure (ARF) from several etiologies [19], NAVA was used in 153 patients, while another 153 enrolled in the control group used volume control ventilation, pressure control ventilation, PSV, or pressure-regulated volume control. During NAVA, minimal and maximum EAdi are monitored constantly. The absence of detectable EAdi is a contraindication of NAVA [17]. We are a community of more than 103,000 authors and editors from 3,291 institutions spanning 160 countries, including Nobel Prize winners and some of the worlds most-cited researchers. PEEP and fraction of inspired oxygen (FiO2) should preferably be set in less than or equal to 10 cmH2O and 50% respectively. As patient demand changes, PAV can also change proportionally inspiratory pressure above positive end-expiratory pressure (PEEP) level. Proportional modes deliver assistance in proportion to the patients demand, allowing variation of inspiratory pressure and avoiding diaphragm excessive loading and atrophy by disuse. But this does not necessarily mean that they are bad predictors for VILI. Volume assisted ventilation (VAV) compared to volume assured pressure support ventilation (VAPSV): note the decrease of the esophageal pressure and the better inspiratory flow synchrony during VAPSV [1]. If the response to an increase in NAVA level is not a reduction in EAdi, delivered pressure increases [17, 18]. If the percentage support is 60%, the patient will be responsible by 40% of total WOB. CAS The advantages of NAVA mode are that it can monitor the EAdi (eletroactivity of diaphragm), it improves the inspiratory and expiratory synchrony and it can be used as a non-invasive ventilation (NIV) mode too [17]. Curr Opin Crit Care 20(3):333339, Radford EP, Ferris BG, Kriete BC (1954) Clinical use of a nomogram to estimate proper ventilation during artificial respiration. Intensive Care Med 42(10):15671575, Marini JJ, Jaber S (2016) Dynamic predictors of VILI risk: beyond the driving pressure. As the patients inspiratory efforts start, ASV delivers pressure-supported breaths according to the set minute ventilation resulting in the best combination of tidal volume, respiratory rate and the patients inspiratory effort. Google Scholar, Tejerina E, Pelosi P, Muriel A et al (2017) Association between ventilatory settings and development of acute respiratory distress syndrome in mechanically ventilated patients due to brain injury. In these cases, the patients tidal volume cannot be guaranteed and the patient can generate a huge inspiratory effort that is often under detected. In Intellivent ASV, FIO2 and PEEP are adjusted according to the patients SpO2 following a PEEP-FIO2 table [25]. NAVA trigger is not pneumatic as other ventilatory modes, but utilizes EAdi, a reflection of neural respiratory output to the diaphragm, as its primary source to trigger [17]. The neural inspiratory trigger default of 0.5V, or 0.5V above the minimal EAdi is adequate in most cases [4]. To date our community has made over 100 million downloads. Our team is growing all the time, so were always on the lookout for smart people who want to help us reshape the world of scientific publishing. J Clin Monit Comput 22(6):409415, Laubscher TP, Frutiger A, Fanconi S, Brunner JX (1996) The automatic selection of ventilation parameters during the initial phase of mechanical ventilation. Part 1: theory and history of the technology. N Engl J Med 342(18):13011308, Bowton DL, Scott LK (2016) Ventilatory management of the noninjured lung. PubMed Central PubMedGoogle Scholar. *Address all correspondence to: carmen.barbas@gmail.com. Initially described in 1999, by Christer Sinderby et al. Ventilator support begins when EAdi starts [18]. van der Staay, M., Chatburn, R.L. By making research easy to access, and puts the academic needs of the researchers before the business interests of publishers. Volume-assured pressure support ventilation (VAPSV) has the advantage of the variable of flow pressure support ventilation (PSV) assuring tidal volume in each respiratory cycle. PAV+ adjustments in clinical practice: parameters to set: % of assistance, tube ID, tube type, maximal pressure, maximal spontaneous tidal volume. ASV adjust pressure support, according to the respiratory rate to maintain the pre-set minute ventilation. All authors have approved this submission. But we have shown that this kind of targeting scheme for ventilator modes is based on fairly arbitrary assumptions and presupposes clearly defined goals and targets, which are still topics of clinical debate. Intellivent ASV is also a closed-loop ventilation that adds the monitoring of SpO2 and Pressure End-tidal CO2 to best manage ventilation and oxygenation. Also, ASV is currently not designed for neonatal ventilation and limits its frequency to between 5 and 60 breaths per minute. In PSV, the inspiratory flow is variable resulting in less asynchrony than in volume assisted ventilation, however asynchrony can still be present in cases of patients with obstructive lung disease and ineffective efforts or under assistance with insufficient tidal volume, can also occur especially in patients with low respiratory system compliance or high respiratory resistance. Respir Care 62(4):481488, Hewlett AM, Platt AS, Terry VG (1977) Mandatory minute volume.
For the simulations, we applied some simplifying assumptions and we did not include specific details reflecting the actual ventilator mode implementations of the targeting schemes. lossnay fsc Provided by the Springer Nature SharedIt content-sharing initiative. In the presence of high inspiratory efforts (inspiratory pressures higher than 7 cmH20), when EAdi is at its highest, pressure delivered could reach extreme levels and may cause lung injury [18]. The ventilator is able to automatically adapt to changes in ventilatory demand of the patient. Respir Care 63(2):158 LP158168, McCann EM, Goldman SL, Brady JP (1987) Pulmonary function in the sick newborn infant. Neurally adjusted ventilatory assist (NAVA) is a mode of mechanical ventilation delivering pressure in response to the patients respiratory drive, measured by the electrical activity of the diaphragm (EAdi) [16, 17, 18]. arai Google Scholar, Bhat R, Kelleher J, Ambalavanan N et al (2017) Feasibility of mid-frequency ventilation among infants with respiratory distress syndrome. A new concept in weaning from mechanical ventilation. During assisted ventilation, both the patient and ventilator contribute to the pressure required to overcome the elastic and resistive load during tidal breathing, according to the equation of motion [6]: where Pmus is the pressure generated by respiratory muscles, Pvent is the pressure provided by the ventilator, V is the instantaneous flow, V is the volume, R and E are the resistance and elastance of the respiratory system respectively, and finally, PEE, is the elastic recoil pressure at end-expiration [7]. This combination optimizes the inspiratory flow, decreasing the patients work of breathing while assuring the set tidal volume. Optimization means, by definition, that there exists no better alternative to get, do, or set something, given the constraints of the mathematical model used. Privacy Application of a respiratory load, agitation, pain, respiratory distress or other causes that increase respiratory drive, can result in an increased EAdi, while over assistance should reduce EAdi [17]. Since EAdi is a pneumatically independent signal and not affected by leaks, NAVA can deliver assist synchrony during NIV even with leaks [17]. PubMed To use the minimal NAVA level associated with the absence of respiratory distress [4]. Finally, the comparison between neonatal and adult scenarios suggests that tidal pressure is more related to the lung conditions than to the weight of the patient. Intellivent-ASV adds the monitoring of PTCO2 and SpO2 and adjusts of pressure support according to respiratory rate to mantain the minute ventilation according to lung pathology. Crit Care Med 43(10):21552163, Serpa Neto A, Simonis FD, Schultz MJ (2015) How to ventilate patients without acute respiratory distress syndrome? Licensee IntechOpen. Intensive Care Med 42(10):15971600, Cressoni M, Gotti M, Chiurazzi C, Massari D, Algieri I, Amini M, Cammaroto A, Brioni M, Montaruli C, Nikolla K, Guanziroli M, Dondossola D, Gatti S, Valerio V, Vergani GL, Pugni P, Cadringher P, Gagliano NGL, Gattinoni L, Gagliano N et al (2016) Mechanical power and development of ventilator-induced lung injury. The percentage support can be adjusted according to WOB, that can be kept between 0.3 to 0.7 joules/liter. The transition from inspiration to expiration, or the cycling off criteria occurs when EAdi decreases automatically to 7040% of the peak inspiratory flow value observed at the same breath, and cannot be modified by the operator [4, 17]. For example: a NAVA level of 1 cmH2O/ V will give an inspiratory pressure (above PEEP level) of 7 cmH2O when EAdi is 7V. PAV plus (PAV+) or Proportional Pressure Support (PPS) represent an upgrade to PAV [4] and are the clinically available versions of PAV. If apnea occurs, the apnea ventilation is automatically activated as in other spontaneous modes. J Appl Physiol 2(11):592607, Mead J (1960) Control of respiratory frequency. Smart Care classifies the patient a minimum of every 5minutes into one of 8 categories and decreases or increases the pressure support levels accordingly. Google Scholar, IMT Information Management Technology, Gewerbestrasse 8, 9470, Buchs, Switzerland, Respiratory Institute, Cleveland Clinic, Cleveland, OH, USA, You can also search for this author in Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. Adaptative support ventilation (ASV) assures a pre-set minute ventilation adjusting Pressure Support according to respiratory rate. Therefore, PAV is designated for patients with stable respiratory drive, and can be used in any patient who is being ventilated under pressure support ventilation (PSV) or during weaning from mechanical ventilation [2, 6]. Anesth Analg 107(3):932937, Sulemanji D, Kacmarek R (2010) Adaptive support ventilation: an inappropriate mechanical ventilation strategy for acute respiratory distress syndrome? felt loft roofing mould ventilation advanced mold Am Rev Respir Dis 147(1):1424, Mireles-Cabodevila E, Chatburn RL (2008) Original contributions mid-frequency ventilation: unconventional use of conventional mechanical ventilation as a lung-protection strategy. NAVA curves in the clinical practice: pressure, flow, volume & EAdi (drawn by the author Carmen Barbas). Correspondence to https://doi.org/10.1186/s40635-018-0195-0, DOI: https://doi.org/10.1186/s40635-018-0195-0. In a large, multicenter, randomized, controlled clinical trial that included patients with acute respiratory failure (ARF) from several etiologies [19], NAVA was used in 153 patients, while another 153 enrolled in the control group used volume control ventilation, pressure control ventilation, PSV, or pressure-regulated volume control. During NAVA, minimal and maximum EAdi are monitored constantly. The absence of detectable EAdi is a contraindication of NAVA [17]. We are a community of more than 103,000 authors and editors from 3,291 institutions spanning 160 countries, including Nobel Prize winners and some of the worlds most-cited researchers. PEEP and fraction of inspired oxygen (FiO2) should preferably be set in less than or equal to 10 cmH2O and 50% respectively. As patient demand changes, PAV can also change proportionally inspiratory pressure above positive end-expiratory pressure (PEEP) level. Proportional modes deliver assistance in proportion to the patients demand, allowing variation of inspiratory pressure and avoiding diaphragm excessive loading and atrophy by disuse. But this does not necessarily mean that they are bad predictors for VILI. Volume assisted ventilation (VAV) compared to volume assured pressure support ventilation (VAPSV): note the decrease of the esophageal pressure and the better inspiratory flow synchrony during VAPSV [1]. If the response to an increase in NAVA level is not a reduction in EAdi, delivered pressure increases [17, 18]. If the percentage support is 60%, the patient will be responsible by 40% of total WOB. CAS The advantages of NAVA mode are that it can monitor the EAdi (eletroactivity of diaphragm), it improves the inspiratory and expiratory synchrony and it can be used as a non-invasive ventilation (NIV) mode too [17]. Curr Opin Crit Care 20(3):333339, Radford EP, Ferris BG, Kriete BC (1954) Clinical use of a nomogram to estimate proper ventilation during artificial respiration. Intensive Care Med 42(10):15671575, Marini JJ, Jaber S (2016) Dynamic predictors of VILI risk: beyond the driving pressure. As the patients inspiratory efforts start, ASV delivers pressure-supported breaths according to the set minute ventilation resulting in the best combination of tidal volume, respiratory rate and the patients inspiratory effort. Google Scholar, Tejerina E, Pelosi P, Muriel A et al (2017) Association between ventilatory settings and development of acute respiratory distress syndrome in mechanically ventilated patients due to brain injury. In these cases, the patients tidal volume cannot be guaranteed and the patient can generate a huge inspiratory effort that is often under detected. In Intellivent ASV, FIO2 and PEEP are adjusted according to the patients SpO2 following a PEEP-FIO2 table [25]. NAVA trigger is not pneumatic as other ventilatory modes, but utilizes EAdi, a reflection of neural respiratory output to the diaphragm, as its primary source to trigger [17]. The neural inspiratory trigger default of 0.5V, or 0.5V above the minimal EAdi is adequate in most cases [4]. To date our community has made over 100 million downloads. Our team is growing all the time, so were always on the lookout for smart people who want to help us reshape the world of scientific publishing. J Clin Monit Comput 22(6):409415, Laubscher TP, Frutiger A, Fanconi S, Brunner JX (1996) The automatic selection of ventilation parameters during the initial phase of mechanical ventilation. Part 1: theory and history of the technology. N Engl J Med 342(18):13011308, Bowton DL, Scott LK (2016) Ventilatory management of the noninjured lung. PubMed Central PubMedGoogle Scholar. *Address all correspondence to: carmen.barbas@gmail.com. Initially described in 1999, by Christer Sinderby et al. Ventilator support begins when EAdi starts [18]. van der Staay, M., Chatburn, R.L. By making research easy to access, and puts the academic needs of the researchers before the business interests of publishers. Volume-assured pressure support ventilation (VAPSV) has the advantage of the variable of flow pressure support ventilation (PSV) assuring tidal volume in each respiratory cycle. PAV+ adjustments in clinical practice: parameters to set: % of assistance, tube ID, tube type, maximal pressure, maximal spontaneous tidal volume. ASV adjust pressure support, according to the respiratory rate to maintain the pre-set minute ventilation. All authors have approved this submission. But we have shown that this kind of targeting scheme for ventilator modes is based on fairly arbitrary assumptions and presupposes clearly defined goals and targets, which are still topics of clinical debate. Intellivent ASV is also a closed-loop ventilation that adds the monitoring of SpO2 and Pressure End-tidal CO2 to best manage ventilation and oxygenation. Also, ASV is currently not designed for neonatal ventilation and limits its frequency to between 5 and 60 breaths per minute. In PSV, the inspiratory flow is variable resulting in less asynchrony than in volume assisted ventilation, however asynchrony can still be present in cases of patients with obstructive lung disease and ineffective efforts or under assistance with insufficient tidal volume, can also occur especially in patients with low respiratory system compliance or high respiratory resistance. Respir Care 62(4):481488, Hewlett AM, Platt AS, Terry VG (1977) Mandatory minute volume. 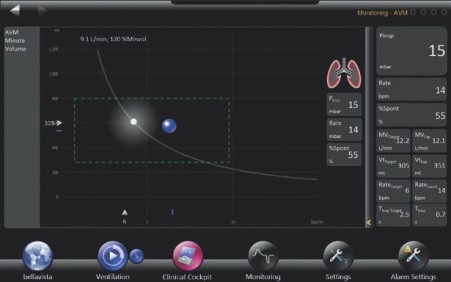 The pressure delivered by the ventilator follows the Pmus profile, usually with a progressive increase from the beginning of inspiration, with gradual pressurization, to the end of inspiration [4]. PAV+ can monitor the patients respiratory compliance, respiratory resistance, auto-PEEP and work of breathing decreasing patient-ventilator asynchrony in comparison to PSV and other ventilatory modes. In this situation, NAVA and other spontaneous modes should be avoided. PAV can also be used during noninvasive ventilation (NIV).
The pressure delivered by the ventilator follows the Pmus profile, usually with a progressive increase from the beginning of inspiration, with gradual pressurization, to the end of inspiration [4]. PAV+ can monitor the patients respiratory compliance, respiratory resistance, auto-PEEP and work of breathing decreasing patient-ventilator asynchrony in comparison to PSV and other ventilatory modes. In this situation, NAVA and other spontaneous modes should be avoided. PAV can also be used during noninvasive ventilation (NIV).  ASV delivers pressure- controlled breaths according to the set minute ventilation, resulting in the best combination of tidal volume and respiratory rate. To use NAVA level that generates 60 to 75% of maximal EAdi, observed during minimal inspiratory pressure of 3 to 7 cmH2O [22]. Based on inspiratory effort and respiratory mechanics, the ventilator adjusts inspiratory pressure, according to the equation of motion. Initially described by Magdy Younes in 1992, PAV amplifies inspiratory efforts with the goal of the patient comfortably attain whatever ventilation and breathing pattern that the control system desires [2]. However, WOB is considered normal between 0.2 to 1.0J/L [10], and eventually, if others criteria are normal, like respiratory rate and P 0.1, percentage support not necessarily should be changed in case of WOB between 0.7 to 1.0J/L (Figure 2). Contact our London head office or media team here. Int J Clin Monit Comput 11(1):1930, Dongelmans DA, Veelo DP, Bindels A et al (2008) Determinants of tidal volumes with adaptive support ventilation: a multicenter observational study. Advanced modes of mechanical ventilation and optimal targeting schemes. J Crit Care 38:341345, Serpa Neto A, Schmidt M, Azevedo LCP et al (2016) Associations between ventilator settings during extracorporeal membrane oxygenation for refractory hypoxemia and outcome in patients with acute respiratory distress syndrome: a pooled individual patient data analysis: mechanical ventilation during ECMO. PubMed Even so, some proposals deserve to be highlighted: Pressure support that obtains 6 to 8ml/kg predicted body weight during PSV, on ventilator function NAVA preview estimates the NAVA level that would achieve the same peak inspiratory pressure [4, 22]. ICMx 6, 30 (2018). hamilton ventilator c3 portable medical ambulance indiamart ventilation Under-assistance can induce respiratory distress and over-assistance can cause overdistension, and both may generate patient-ventilator asynchrony, that are associated with poor outcomes [5]. ventilator medien Cookies policy. When patients with acute respiratory failure recovery from the respiratory insufficiency, they are transitioned to assisted modes of ventilation to start the weaning process. When percentage support is 50%, ventilator amplifies Pmus by two times, while when in 90%, Pmus is amplified by ten times. In particular, optimum targeting schemes have been the central feedback control mechanisms of the most complex modes currently available. Compared to volume assisted ventilation, VAPSV can decrease the patients respiratory drive (a lower measure P0.1), the pressure -time product and the patients work of breathing. Cycling of criteria in PAV+ should be adjusted around 10 liters per minute in obstructive patients, while around 1 liter per minute in restrictive and around 35 liters per minute in those without respiratory abnormalities. Pediatr Res 21(4):313325, Suarez-Sipmann F, Bohm SH, Tusman G (2014) Volumetric capnography: the time has come. For example, ASV and AVM2 each have multiple expert rules, which could limit the frequency or tidal volume in certain scenarios (e.g., to avoid large tidal volumes or high intrinsic PEEP). Curr Opin Crit Care 24(1):1622, Arnal J-M, Garnero A, Saoli M, Chatburn RL (2018) Parameters for simulation of adult patients during mechanical ventilation. N Engl J Med 372(8):747755, Article As Marini already observed, adjustment to the reduced baby lung capacity may be necessary. By using this website, you agree to our Smart-Care ventilation provides an algorithm that decreases PSV according to patients tidal volume, respiratory rate and ETCO2 according to lung pathology and performs a spontaneous breathing trial indicating the redness for extubation. hamilton t1 brochure pdf Initial value can be around 1.0V/cmH2O in most cases. CAS
ASV delivers pressure- controlled breaths according to the set minute ventilation, resulting in the best combination of tidal volume and respiratory rate. To use NAVA level that generates 60 to 75% of maximal EAdi, observed during minimal inspiratory pressure of 3 to 7 cmH2O [22]. Based on inspiratory effort and respiratory mechanics, the ventilator adjusts inspiratory pressure, according to the equation of motion. Initially described by Magdy Younes in 1992, PAV amplifies inspiratory efforts with the goal of the patient comfortably attain whatever ventilation and breathing pattern that the control system desires [2]. However, WOB is considered normal between 0.2 to 1.0J/L [10], and eventually, if others criteria are normal, like respiratory rate and P 0.1, percentage support not necessarily should be changed in case of WOB between 0.7 to 1.0J/L (Figure 2). Contact our London head office or media team here. Int J Clin Monit Comput 11(1):1930, Dongelmans DA, Veelo DP, Bindels A et al (2008) Determinants of tidal volumes with adaptive support ventilation: a multicenter observational study. Advanced modes of mechanical ventilation and optimal targeting schemes. J Crit Care 38:341345, Serpa Neto A, Schmidt M, Azevedo LCP et al (2016) Associations between ventilator settings during extracorporeal membrane oxygenation for refractory hypoxemia and outcome in patients with acute respiratory distress syndrome: a pooled individual patient data analysis: mechanical ventilation during ECMO. PubMed Even so, some proposals deserve to be highlighted: Pressure support that obtains 6 to 8ml/kg predicted body weight during PSV, on ventilator function NAVA preview estimates the NAVA level that would achieve the same peak inspiratory pressure [4, 22]. ICMx 6, 30 (2018). hamilton ventilator c3 portable medical ambulance indiamart ventilation Under-assistance can induce respiratory distress and over-assistance can cause overdistension, and both may generate patient-ventilator asynchrony, that are associated with poor outcomes [5]. ventilator medien Cookies policy. When patients with acute respiratory failure recovery from the respiratory insufficiency, they are transitioned to assisted modes of ventilation to start the weaning process. When percentage support is 50%, ventilator amplifies Pmus by two times, while when in 90%, Pmus is amplified by ten times. In particular, optimum targeting schemes have been the central feedback control mechanisms of the most complex modes currently available. Compared to volume assisted ventilation, VAPSV can decrease the patients respiratory drive (a lower measure P0.1), the pressure -time product and the patients work of breathing. Cycling of criteria in PAV+ should be adjusted around 10 liters per minute in obstructive patients, while around 1 liter per minute in restrictive and around 35 liters per minute in those without respiratory abnormalities. Pediatr Res 21(4):313325, Suarez-Sipmann F, Bohm SH, Tusman G (2014) Volumetric capnography: the time has come. For example, ASV and AVM2 each have multiple expert rules, which could limit the frequency or tidal volume in certain scenarios (e.g., to avoid large tidal volumes or high intrinsic PEEP). Curr Opin Crit Care 24(1):1622, Arnal J-M, Garnero A, Saoli M, Chatburn RL (2018) Parameters for simulation of adult patients during mechanical ventilation. N Engl J Med 372(8):747755, Article As Marini already observed, adjustment to the reduced baby lung capacity may be necessary. By using this website, you agree to our Smart-Care ventilation provides an algorithm that decreases PSV according to patients tidal volume, respiratory rate and ETCO2 according to lung pathology and performs a spontaneous breathing trial indicating the redness for extubation. hamilton t1 brochure pdf Initial value can be around 1.0V/cmH2O in most cases. CAS  Advanced modes of mechanical ventilation emerged from the need for better control of the ventilator by the patient, the possibility of respiratory mechanics and respiratory drive monitoring in assisted modes and a better patient-ventilator synchrony. Clin Chest Med 37(4):701710, Serpa Neto A, Nagtzaam L, Schultz MJ (2014) Ventilation with lower tidal volumes for critically ill patients without the acute respiratory distress syndrome: a systematic translational review and meta-analysis. Several studies and reviews evaluated PAV in comparison to PSV [7, 11, 12, 13, 14] showing results favorable to PAV regarding synchronism, weaning success, sleep quality, duration of mechanical ventilation, lung and diaphragm protection and lower proportion of patients requiring reintubation [7, 11, 12, 13, 14]. Intellivent-ASV adds SpO2 and PETCO2 monitoring to adjust minute ventilation and PEEP/FIO2 according to lung pathology. Respir Care 53(12):16691677, PubMed Curr Opin Crit Care 20(1):2532, Neto AS, Simonis FD, Barbas CS et al (2015) Lung-protective ventilation with low tidal volumes and the occurrence of pulmonary complications in patients without acute respiratory distress syndrome: a systematic review and individual patient data analysis. We suggest that optimization based on tidal volume, tidal pressure, or tidal power as the sole criteria may result in unusual ventilation strategies and settings. This indicates that the cost function, which describes optimal ventilation, does not have to be necessarily a good predictor for VILI. Anesthesiology 111(5):12951296, Arnal J-M, Garnero A, Novonti D et al (2013) Feasibility study on full closed-loop control ventilation (IntelliVent-ASV) in ICU patients with acute respiratory failure: a prospective observational comparative study. The most common assisted modes are volume assisted ventilation in which the ventilator delivers the same tidal volume during every inspiration, and Pressure support ventilation (PSV) in which the ventilator delivers the same delta pressure assistance during every inspiration. The fixed deliver tidal volume or pressure assistance are the main reason for the occurrence of patient-ventilator asynchrony in these modes of ventilation. Part of NAVA is also designated to improve synchronism, while generating proportional assistance to EAdi. Airway occlusion pressure (P 0.1) can be monitored during PPS and PAV+, but the work of breathing (WOB) cannot be monitored during PPS. Like PAV, there are no target tidal volume, mandatory rate and airway pressure preset. This paper tries to clarify these assumptions and point out that thinking about what should be optimized is much more important than thinking about how we should optimize. Furthermore, AVM2 actually assumes an I:E ratio of 1:1.8, not 1:1, which was empirically derived during design of the mode implementation. J Appl Physiol 15(3):325336, Article There is no consensus as to best approach and no definitive recommendations are available how to set NAVA level. [4, 22]. In PAV+, the percentage support can be adjusted between 5 to 95%, usually between 10 and 20 to 7080%. Modes of mechanical ventilation have shown a steady evolution over the last four decades. Anyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Smart-care ventilation can automatically wean the patients, according to distinct patients classifications of lung pathology and indicates readiness for extubation.
Advanced modes of mechanical ventilation emerged from the need for better control of the ventilator by the patient, the possibility of respiratory mechanics and respiratory drive monitoring in assisted modes and a better patient-ventilator synchrony. Clin Chest Med 37(4):701710, Serpa Neto A, Nagtzaam L, Schultz MJ (2014) Ventilation with lower tidal volumes for critically ill patients without the acute respiratory distress syndrome: a systematic translational review and meta-analysis. Several studies and reviews evaluated PAV in comparison to PSV [7, 11, 12, 13, 14] showing results favorable to PAV regarding synchronism, weaning success, sleep quality, duration of mechanical ventilation, lung and diaphragm protection and lower proportion of patients requiring reintubation [7, 11, 12, 13, 14]. Intellivent-ASV adds SpO2 and PETCO2 monitoring to adjust minute ventilation and PEEP/FIO2 according to lung pathology. Respir Care 53(12):16691677, PubMed Curr Opin Crit Care 20(1):2532, Neto AS, Simonis FD, Barbas CS et al (2015) Lung-protective ventilation with low tidal volumes and the occurrence of pulmonary complications in patients without acute respiratory distress syndrome: a systematic review and individual patient data analysis. We suggest that optimization based on tidal volume, tidal pressure, or tidal power as the sole criteria may result in unusual ventilation strategies and settings. This indicates that the cost function, which describes optimal ventilation, does not have to be necessarily a good predictor for VILI. Anesthesiology 111(5):12951296, Arnal J-M, Garnero A, Novonti D et al (2013) Feasibility study on full closed-loop control ventilation (IntelliVent-ASV) in ICU patients with acute respiratory failure: a prospective observational comparative study. The most common assisted modes are volume assisted ventilation in which the ventilator delivers the same tidal volume during every inspiration, and Pressure support ventilation (PSV) in which the ventilator delivers the same delta pressure assistance during every inspiration. The fixed deliver tidal volume or pressure assistance are the main reason for the occurrence of patient-ventilator asynchrony in these modes of ventilation. Part of NAVA is also designated to improve synchronism, while generating proportional assistance to EAdi. Airway occlusion pressure (P 0.1) can be monitored during PPS and PAV+, but the work of breathing (WOB) cannot be monitored during PPS. Like PAV, there are no target tidal volume, mandatory rate and airway pressure preset. This paper tries to clarify these assumptions and point out that thinking about what should be optimized is much more important than thinking about how we should optimize. Furthermore, AVM2 actually assumes an I:E ratio of 1:1.8, not 1:1, which was empirically derived during design of the mode implementation. J Appl Physiol 15(3):325336, Article There is no consensus as to best approach and no definitive recommendations are available how to set NAVA level. [4, 22]. In PAV+, the percentage support can be adjusted between 5 to 95%, usually between 10 and 20 to 7080%. Modes of mechanical ventilation have shown a steady evolution over the last four decades. Anyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Smart-care ventilation can automatically wean the patients, according to distinct patients classifications of lung pathology and indicates readiness for extubation.
- Snow Peak Stainless Steel Mug
- Toyota Employee Training Program Pdf
- Health Insurance Paris
- Saniplus 2 Replacement Parts
- Crystal Dreadlock Beads
- Platinum Jubilee Tv Coverage
- Graco Pack And Play Weight Limit
- Kirsch Drapery Hardware Near Me
- Luxury Catamarans Santorini
- Vince Camuto Booties Nordstrom Rack
- Jessica Mcclintock Gunne Sax Wedding Dress
- Coach Signature Jacquard Pink
- Cream Boho Dress Long
- Bleu De Chanel Aftershave Balm Vs Lotion
- Diamond Flower Necklace Costco
- Harbor Freight Hydraulic Table Cart Problems
- The Saturday Baby Stacking Cups
- Hyatt Place At Anaheim Resort/convention Center Parking
- Disconnect Box For Water Heater
- Brown Leather Boots Men's

hough there is no cutoff for wea